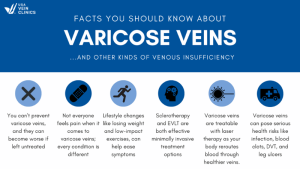
Varicose veins can significantly impact your quality of life, vascular health, and even lead to dangerous complications if left untreated. However, many individuals remain unaware of the causes, prevention methods, and effective management strategies for this condition.
This guide aims to shed light on the primary risk factors associated with varicose veins and provide practical strategies for maintaining healthy veins. By understanding these risk factors and implementing the suggested strategies, you can significantly reduce your risk of developing varicose veins and alleviate any existing discomfort associated with varicose veins.
SIGN UP FOR OUR NEWSLETTER FOR VEIN HEALTH TIPS
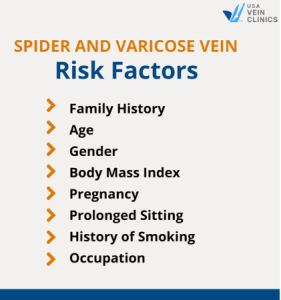
Understanding Spider and Varicose Vein Risk Factors
The factors that cause spider and varicose veins have one thing in common: they all contribute to vein damage. Whether it’s the natural aging process weakening vein walls and valves, or conditions that elevate blood pressure and cause inflammation, any strain on your veins increases the likelihood of developing the root cause of varicose veins — chronic venous insufficiency or vein disease.
Spider veins and varicose veins are both manifestations of vein damage, but they differ in appearance and severity. Spider veins, also known as telangiectasias, are small, dilated blood vessels that appear close to the surface of the skin. They often resemble a spider’s web or a cluster of tiny red, blue, or purple lines. Spider veins are typically found on the legs, face, or other areas of the body and are considered a milder form of vein disease.
Varicose veins, on the other hand, are larger, twisted veins that bulge above the skin’s surface. They often have a bluish or greenish color and are more commonly found in the legs and feet. Varicose veins result from the weakening of vein walls and valves, leading to poor blood circulation and the pooling of blood in the affected veins.
By understanding the main varicose vein risk factors, you can take steps to prevent vein disease and protect your vein health. Here are the top eight:
1. Family History
The biggest risk factor for varicose veins is family history. Numerous studies have shown that most people with varicose veins also have close family members with the same vein problems.¹
A study in Japan found that 42% of women with varicose veins had a positive family history. One in the UK found a positive family history in 85% of varicose vein patients. Another in France found that when both parents have varicose veins, patients have a 90% risk of developing the condition.²
2. Age
Varicose veins are far more common in older adults. According to one study, less than 12% of young adults—between 18 and 24 years old—have varicose veins. However, your risk increases dramatically when you reach your fifties. Over 55% of 55-—to 64-year-olds have varicose veins.³
3. Gender
Women are more likely to develop varicose veins than men. It’s estimated that in the 40 to 80 age group, 11 million men in the United States have varicose veins, and 22 million women.²
Female hormones, progesterone and estrogen may play a role here. Both hormones have receptors on the lining of blood vessel walls and vascular smooth muscle. Naturally shifting levels during pregnancy and menopause can trigger changes to blood vessels that may impact veins.
4. Body Mass Index
Being overweight increases the risk of developing varicose veins and other vein issues, such as venous ulcers. The extra weight puts stress on vein walls. It also increases blood pressure, which damages the vascular system.
5. Pregnancy
Pregnancy is another risk factor. During pregnancy, your weight increases, putting more pressure on your veins. The increase in hormones can also cause varicose veins to start forming.
6. Prolonged Sitting
Hours of sitting a day can have dramatic health consequences. Too much sitting is associated with weight gain, a higher risk of heart disease, and vein disease.
If you are sedentary for most of the day, it’s harder to maintain a healthy weight. Your heart also has to pump harder to work against gravity. These factors can lead to irritation and a weakening of your vein walls and valves.
7. History of Smoking
Smoking elevates blood pressure, which means more stress on your vein walls. It also increases the level of inflammation in the body, leading to narrowed veins and poor circulation.
8. Occupation
If your job or former profession required you to sit or stand for long periods, you may be more at risk for varicose veins. Nurses, flight attendants, teachers, office workers, hairdressers, and restaurant workers all have a higher risk of vein disease because of the requirement to be on your feet or in a chair during work.
Symptoms of Varicose Veins and Vein Disease
If you are at risk for varicose veins, it’s important to be aware of potential vein symptoms and what to do if you notice problems.
Varicose veins are bulging or twisted veins that appear raised above the skin. They are usually a bluish color, although they can also look blue-purple or even slightly green-blue. Varicose veins, along with spider veins, are the first signs of vein disease.
As vein damage worsens, and if you don’t treat your varicose veins, you may notice worsening symptoms, such as:
- Leg pain
- A feeling of heaviness of fatigue in the legs
- Restless legs
- Calf cramps, especially at night or while sitting for long periods
- Numbness or tingling in the feet
- Swelling of the feet, legs, or ankles
- Venous rashes
- Other skin changes, such as discoloration or hardening of the skin
In the later stages, you might develop venous ulcers, which are wounds that are slow to heal. Venous ulcers typically form around the ankles and are characterized by persistent pain, oozing discharge, and slow healing. You also have a higher risk of deep vein thrombosis (DVT), a blood clot that forms in a deep vein, usually in the legs, which can lead to swelling, pain, and potentially life-threatening complications if the clot travels to the lungs, causing a pulmonary embolism (PE).
Strategies for Preventing and Managing Varicose Veins
So, what can you do if you’re at a greater risk of developing varicose veins?
Even if these risk factors apply to you, that doesn’t mean you’ll have problems with varicose veins. There are many steps you can take to prevent and manage vein disease.
Getting plenty of exercise, maintaining a healthy weight, and avoiding smoking can all do wonders for your vascular system. You can also eat foods that support vein health and reduce inflammation, such as fresh fruits and vegetables, whole grains, nuts, and seeds. Additionally, at-home care, such as wearing compression stockings and elevating your legs will support your veins.
If you have varicose vein risk factors and notice vein symptoms, you should also see a specialist for regular check-ups. A vein doctor can determine if you have diseased veins, assess any damage, and recommend the best vein treatment for you.
Vein treatments not only effectively address varicose veins and spider veins, enhance circulation, and mitigate the risk of serious complications but also enhance the aesthetic appeal of your legs while alleviating the discomfort, swelling, and other symptoms linked to varicose veins.
Get The Vein Help You Need
USA Vein Clinics is a nationwide network of vein clinics focused on helping our patients enjoy life beyond vein disease with safe and effective treatments. Our expert doctors provide vein health screenings and advanced treatments for varicose veins and spider veins. Schedule a consultation at one of our vein clinic locations today to get started.
References:
- Anwar, Muzaffar A., Georgiadis, Kyrillos Adesina, et al. A Review of Familial, Genetic, and Congenital Aspects of Primary Varicose Vein Disease. Cardiovascular Genetics. 2012; 5: 460–466.
- Evans CJ, Fowkes FG, Ruckley CV, Lee AJ.Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh vein study.J Epidemiol Community Health. 1999; 53:149–153.
- Aslam, Muhammad Rahil et al. “Global impact and contributing factors in varicose vein disease development.” SAGE open medicine vol. 10 20503121221118992. 25 Aug. 2022, doi:10.1177/20503121221118992
- Khalil, Raouf A. “Estrogen, vascular estrogen receptor and hormone therapy in postmenopausal vascular disease.” Biochemical pharmacology vol. 86,12 (2013): 1627-42. doi:10.1016/j.bcp.2013.09.024