May-Thurner Syndrome: Symptoms, Causes, and Treatment
If you have ever experienced Deep Vein Thrombosis (DVT) or any unusual swelling in your left leg, you may benefit from talking to a vein specialist about May-Thurner syndrome (MTS). Although rare, May-Thurner syndrome often remains undiagnosed, leading to serious health consequences.
Below, we discuss everything you need to know about May-Thurner syndrome: what it is, why it develops, how it is diagnosed, and what treatment options are available. At USA Vein Clinics, our board-certified vein specialists can evaluate May-Thurner syndrome, venous symptoms
What Is May-Thurner Syndrome?
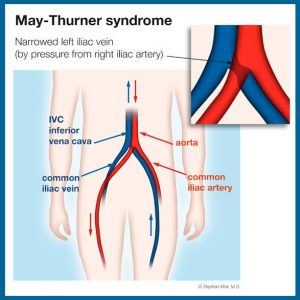
May-Thurner syndrome, also known as iliac vein compression syndrome, occurs when the right iliac artery compresses the left iliac vein. This can cause the left leg to swell, along with increasing your risk for deep vein thrombosis.
Although they are not always present in patients, May-Thurner syndrome symptoms can include:
- Leg swelling
- Venous ulcers
- Unusual sensations like itching or burning
May-Thurner syndrome often remains undiagnosed until deep vein thrombosis develops.
DVT is a blood clot in the deep venous system or veins located deep within your body. It is a serious medical condition because if the blood clot, or a piece of the blood clot, breaks free and travels to the lungs, it can cause a blockage in one of the pulmonary arteries. This condition, known as pulmonary embolism, can be life-threatening and requires immediate medical treatment. It is important to be familiar with common signs of DVT and pulmonary embolism to prevent venous complications. Symptoms of DVT include:
- Swelling in the leg (or less frequently, the arm)
- Warmth when you touch the affected area
- Skin redness on the legs
- Pain or tenderness in your lower body, such as a cramp
Although DVT can occur almost anywhere in the body, usually only one side is affected. If you experience any DVT symptoms, you should contact your doctor immediately or seek urgent medical care.
Symptoms of pulmonary embolism include:
- Sudden shortness of breath
- Chest pain
- Dizziness
- Coughing
- Sweating
If you experience signs of pulmonary embolism, be sure to call 911 immediately or go directly to the nearest emergency room.
May-Thurner Syndrome Causes
To better understand why May-Thurner syndrome occurs, familiarization with the roles of the iliac artery and the iliac vein may help. The iliac artery, located near the pelvis, is responsible for carrying oxygen-rich blood from the heart to the back and other regions of the body. The iliac vein, located in the abdomen, is responsible for transporting blood from the pelvis and lower limbs back to the heart for reoxygenation.
May-Thurner syndrome develops when the iliac artery compresses the iliac vein, restricting blood flow from the left leg. This can cause left leg swelling and increase your risks of developing DVT and pulmonary embolism.
Although it is unclear how many people suffer from May-Thurner syndrome, it may be responsible for two to five percent of all DVT cases.
Research indicates an estimated prevalence rate found at autopsy is as high as 22-32 percent.[1]
May-Thurner Syndrome Risk Factors
Most often, May-Thurner syndrome affects younger women, between the ages of 20 and 40. Pregnancy, as well as long periods of inactivity, can impact your risk of developing MTS.
Unfortunately, MTS does not usually come with warning signs or symptoms. Therefore, you should keep an eye out for unexplained leg swelling, along with other symptoms of DVT.
Risk factors that increase your risk of DVT include:
- Recent surgery or injury: Trauma, surgery, and infection can damage your veins and increase the risk of developing blood clots.
- Blood-clotting disorder: If you or someone in your family has a blood clotting disorder or a history of blood clots, you are at higher risk for future problems.
- Extended stretches of inactivity: Long periods of inactivity, such as air or car travel, can impact blood flow, placing you at increased risk for DVT.
- Smoking: Smoking can affect circulation and blood clotting, increasing the risk of deep vein thrombosis.
- Cancer: Some types of cancer, along with cancer treatments like chemotherapy, can make you more likely to develop blood clots.
- Obesity: Obesity or being overweight can strain your veins, increasing your risk of deep vein thrombosis.
- Pregnancy: Your expanding uterus, along with pregnancy-related weight gain, can increase pressure on veins in your legs, making DVT more likely to occur.
- Age: Although anyone of any age can develop DVT, your risk elevates as you get older.
- Varicose veins: Having varicose veins and other varicosities may elevate your risk for blood clots.
We also want you to know that varicose veins are caused by underlying vein disease or venous insufficiency. Vein disease is another risk factor for deep vein thrombosis. It develops when vein valves become damaged and begin to malfunction. This often leads to blood pooling in the legs, ankles, and feet.
Common vein disease symptoms include:
- Swelling in your legs and ankles
- Cramping or aching in the thigh or calf
- Tired or heavy legs
- Restlessness, especially at night
- Itchy, dry, or hardened skin on your legs
- Wounds on your legs or ankles that take a long time to heal or don’t heal at all
- Leg pain that is alleviated when you walk or elevate your legs
For a full evaluation of your vein health, we recommend contacting an experienced vein specialist. When vein disease is left untreated, it can place you at increased risk for dangerous conditions. At USA Vein Clinics, we offer consultations to diagnose your vein disease symptoms.
May-Thurner Syndrome Diagnosis
Obtaining a May-Thurner syndrome diagnosis can be challenging. This is because in many cases, there are no symptoms. However, you should be on the lookout for the most common sign of MTS: deep vein thrombosis.
If your doctor suspects you have May-Thurner syndrome, they will perform a physical examination and ask about your medical history. Then, they may order imaging exams to determine whether your right iliac artery compresses your left iliac vein.
Potential imaging exams for May-Thurner syndrome diagnosis include:
- CT: This type of scan uses x-rays and a computer to produce images from deep within the body.
- MRI: Magnetic fields and radio waves can generate images of organs and internal soft tissues.
- Ultrasound: An ultrasound uses high-frequency sound waves to view your body’s internal structures.
- Venogram: This form of imaging combines an x-ray and a special dye to obtain imaging of the veins.
Your doctor may also order a catheter-based venogram or intravascular ultrasound. This can help them see inside the blood vessel.
WHAT A LEG ULTRASOUND CAN REVEAL ABOUT YOUR VARICOSE VEINS
May-Thurner Syndrome Treatment Options
May-Thurner syndrome treatment can vary depending on your symptoms and their severity. Some individuals with MTS may benefit from treatment to improve blood flow in the left iliac vein. Vein treatment can also help ease symptoms, along with reducing your risk for DVT.
MTS’s potential treatment options include:
- Venous angioplasty and stenting: In this minimally invasive procedure, a specialist inserts a catheter with a balloon on its tip into your vein. Then, they inflate the balloon to open the vein fully. Next, a tiny mesh tube, called a stent, is inserted to keep the vein open and promote better blood flow. Afterward, the balloon is removed.
- Bypass surgery: In some cases, surgery may be recommended. A bypass graft can reroute blood around the compressed portion of your iliac vein.
- Repositioning: Your doctor may be able to move the right iliac artery behind the left iliac vein. This can remove pressure on the vein, alleviate symptoms, and help prevent DVT.
If you develop deep vein thrombosis due to May-Thurner syndrome, your doctor may prescribe blood thinners, clot-busting medications, or other treatments.
May-Thurner Syndrome Treatment at USA Vein Clinics
At USA Vein Clinics, we perform minimally invasive, office-based treatment for a range of venous conditions, including May-Thurner syndrome. Our vein specialists can provide personalized treatment recommendations at over 100 clinic locations nationwide for your convenience.
Vein treatment is usually covered by most major insurance plans, including Medicare and Medicaid. To discuss the details of your individual plan, just give us a call at 888.768.3467.
To get started on your journey towards better vein health, go ahead and schedule an initial consultation online today.
[1] “May-Thurner Syndrome: