What Is Deep Vein Thrombosis and What Causes It?
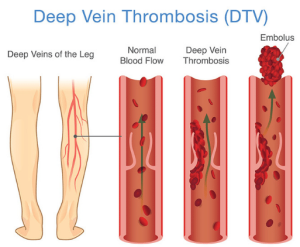
Deep vein thrombosis (DVT) occurs when a blood clot forms in the deep venous system, which is the veins deep within the body, away from the skin’s surface. DVT is most common in the legs but can also develop in the pelvis or arms. Without treatment, DVT can lead to a life-threatening condition called pulmonary embolism.
A pulmonary embolism occurs when a piece of a blood clot breaks away and travels through the bloodstream. This blood clot is called an embolism. If an embolism stemming from deep vein thrombosis reaches the lungs through the bloodstream, it can obstruct blood flow, creating a medical emergency that requires immediate treatment. DVT can also cause longer-term complications, including chronic pain, skin discoloration, and venous ulcers.
Sign Up for Our Newsletter to Learn More About Protecting Your Veins
Deep Vein Thrombosis Symptoms
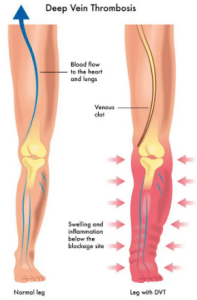
Deep vein thrombosis symptoms can cause excessive pain and impact mobility. This condition can be challenging to diagnose without medical imaging since many deep vein thrombosis symptoms can resemble those of varicose veins. However, symptoms of deep vein thrombosis commonly occur on only one side of the body, typically in one leg or arm.
Some common symptoms of deep vein thrombosis include:
- Leg swelling on one side
- Warmth in the affected area
- Skin redness
- Pain, tenderness, or cramping in the lower extremities
Many individuals don’t notice they have DVT until an embolism reaches the lungs, causing a pulmonary embolism. Symptoms of a pulmonary embolism (PE) include:
- Sudden shortness of breath
- Chest pain that worsens when you take a deep breath
- Dizziness
- Rapid breathing
- Rapid heart rate
If you suspect you have DVT or a pulmonary embolism, we recommend scheduling an appointment with a medical provider to discuss your deep vein thrombosis treatment options. Deep vein thrombosis treatment often involves blood-thinning medications and, in rare instances, surgical intervention.
Deep Vein Thrombosis Risk Factors
There are many potential causes and risk factors for DVT. If you’re worried about developing deep vein thrombosis symptoms, we recommend scheduling an appointment with an experienced vein doctor. They can help identify your individual risks, recommend beneficial lifestyle changes, and closely monitor you for signs of DVT.
Some common risk factors include:
- A recent accident or surgery: DVT can develop in veins damaged by surgery or injury, especially when lengthy bed rest is required.
- Personal or family history: If you, a parent, or a sibling has ever been diagnosed with DVT or another blood-clotting disorder, you are considered at increased risk for venous issues.
- Prolonged sitting: Long periods of sitting, such as during air or car travel, can impact circulation and cause DVT in the lower legs.
- Smoking: Smoking can damage your veins, impact circulation, and lead to dangerous blood clots.
- Varicose veins: Individuals with enlarged, visible leg veins may be at increased risk for developing deep vein thrombosis.
- Cancer: Some types of cancer, including breast, ovarian, pancreatic, bowel, and lung, along with chemotherapy treatment, can make you more likely to develop DVT.
- Obesity: A high body mass index (BMI) can strain your veins, impacting blood flow and increasing the risk for deep vein thrombosis.
- Pregnancy: Women who are pregnant or have recently given birth are at increased risk for DVT due to the expanding uterus placing pressure on surrounding veins, increased blood flow, and damaged vessels after childbirth.
- Aging: Although anyone can develop DVT, your risk increases beyond the age of 40.
- Increased estrogen: High levels of estrogen caused by birth control pills, hormone replacement therapy, or pregnancy can increase your risk of a clot.
Preventing Deep Vein Thrombosis
The good news is that DVT is preventable. There are steps you can take to reduce your risk of developing deep vein thrombosis:
- Move more frequently: Since blood clots often form while traveling or in those who stand or sit for long periods, moving around at least every two hours can help reduce your risk.
- Exercise regularly: Along with avoiding prolonged sitting and standing, it is important to exercise regularly. You should aim for at least 30 minutes a day, 5 days a week. Be sure to consult your doctor before getting started.
- Wear loose-fitting clothing: Tight-fitting clothing can put pressure on your veins, impacting circulation to the legs. Consider switching to loose-fitting clothing, especially when traveling or sitting for prolonged periods.
- Maintain a healthy weight: Losing extra weight can alleviate pressure on your veins, lowering your risk for DVT.
- Quit smoking: Smoking and other tobacco products can cause damage to your blood vessels. If you need help, ask your doctor about smoking cessation programs.
- Wear prescribed compression stockings: Medical-grade compression stockings can alleviate symptoms of deep vein thrombosis, boost circulation, and reduce your risk of developing additional venous issues.
- Review your medications: Certain medications may increase your risk for DVT. Discuss the pros and cons of your medications with your doctor.
- Treat underlying vein disease: If you have vein disease, minimally invasive vein treatment may help reduce your risk of deep vein thrombosis.
Improve Your Vein Health at USA Vein Clinics
To prevent deep vein thrombosis, we encourage you to take control of your vein health and to treat any underlying vein disease. Vein disease can increase your risk of developing DVT. If you have varicose veins, spider veins, or other common symptoms of vein disease, consider scheduling an appointment with a veins specialist to discuss treatment plans and prevention tips.
At USA Vein Clinics, our vein specialists will examine your veins for signs of damage. We offer comprehensive vein health screenings using ultrasound mapping. After your exam, we’ll create a personalized treatment plan to help restore your vein health and reduce your risk of deep vein thrombosis.