Everything You Need to Know About Vein Disease
What is vein disease? This common health condition, also known as chronic venous insufficiency, is the underlying cause of varicose veins, spider veins, reticular veins, and restless leg syndrome (RLS). Results across studies suggest that in the general population, up to 17% of men and up to 40% of women may experience chronic venous insufficiency.
If left untreated, vein disease can cause varicose and spider veins. It can also lead to a range of painful symptoms and place you at increased risk for several serious health conditions, including blood clots and venous ulcers.
Unfortunately, vein disease doesn’t go away on its own. It is a progressive condition, meaning that symptoms usually get worse over time. Fortunately, help is available. At USA Vein Clinics, we specialize in the treatment of vein disease.
Below, we share important information about the symptoms, causes, and risk factors of venous disease. If you have concerns about your vein health, we recommend visiting a vein specialist.
Understanding Vein Disease
To better understand vein disease, it may be helpful to review how the circulatory system works. On a basic level, your circulatory system is made up of the heart and the blood vessels (including arteries and veins) throughout the entire body. Arteries are responsible for transporting oxygenated blood from the heart to the entire body. Then your veins get to work, carrying depleted blood back to the heart for re-oxygenation.
There are two main types of veins in the body: superficial veins (those located close to the skin) and deep veins, which are located deep within the muscle. The deep venous system transports blood to a major vein called the vena cava, which then carries it straight up to the heart.
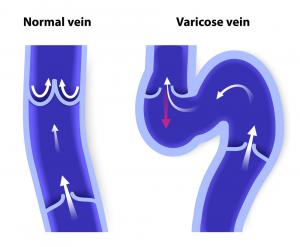
In healthy veins, tiny one-way valves keep blood flowing in the direction of the heart. As you walk or engage in other types of physical activity, your muscles contract around the deep veins in your legs to help push de-oxygenated blood against gravity back to the heart. When you are at rest, your vein valves close to prevent blood from going the wrong way.
In unhealthy veins, these one-way valves become damaged and allow blood flow to leak backward, leading to the development of vein disease.
Symptoms of Vein Disease
Common vein disease symptoms include:
- Swelling in the legs, ankles, and feet
- Tired, aching legs
- Burning in the calf or thigh
- Leg pain that improves with walking or elevation
- Itchy, dry skin
- Numbness or tingling sensations
- Difficulty standing for prolonged periods
- Open, non-healing leg wounds
- Varicose veins and spider veins
If you have visible veins, leg pain, or other signs of venous disease, it is important to seek medical evaluation. A vein specialist can make personalized treatment recommendations that can alleviate symptoms and prevent the progression of the disease.
What Causes Vein Disease?
Over time, vein valves can become strained, which can lead to a condition called venous insufficiency. This involves blood flowing backward or pooling in your legs, ankles, and feet. To accommodate increased blood to the region, veins may begin to expand and eventually develop into varicose veins.
Genetics, aging, and lifestyle factors can contribute to the development of vein disease. To help prevent this challenging condition, we recommend discussing your individual risk factors with a vein specialist.
If you are experiencing signs of venous insufficiency like the appearance of varicose and spider veins, we recommend consulting a vein specialist.
Vein Disease Risk Factors
There are many factors that lead to the development of vein disease. Some of these may be managed with lifestyle changes, however, treatment from a vein specialist is the best way to care for venous insufficiency.
Common risk factors for vein disease include:
- Genetics: If one or both of your parents have varicose veins, you are considered at increased risk. Although you can not control your genes, you may be able to mitigate some of your other risk factors.
- Age: As you grow older, veins tend to weaken and become more susceptible to venous issues. Although vein disease is more common in adults over age 50, individuals of any age can be affected.
- Sex: Women are four times more likely than men to develop varicose veins. This may be partially due to pregnancy, since hormonal influx, weight gain, and increased blood volume are contributing factors.
- Body Mass Index (BMI): Being obese or overweight places additional pressure on your veins, which can lead to their expansion. Maintaining a healthy BMI can lower your risk of developing venous insufficiency.
- Smoking: Smoking can weaken veins, impact blood circulation, and affect your overall health.
- Underlying health conditions: Some health conditions, including high blood pressure and diabetes, may increase your risk of developing vein disease. To reduce your risks, work with your doctor to control these underlying issues.
- Long periods of standing or sitting: Standing or sitting for prolonged periods of time impacts circulation and can lead to vein disease. If you spend a lot of time in one position, consider wearing compression socks and taking frequent breaks to move around.
- Inactivity: Not getting enough exercise can lead to venous disease. Most individuals will benefit from getting at least 30 minutes of physical activity per day, five days a week. However, be sure to talk to your doctor before getting started.
If you are at risk of developing vein disease, you may want to visit a vein specialist. At USA Vein Clinics, our vein specialists make personalized recommendations based on your level of risk and condition to determine the best care plan for improving your quality of life.
How Serious Is Vein Disease?
Vein disease can have serious consequences if left untreated. Common symptoms like cramping and swelling in the legs can impact mobility and quality of life.
We also want you to know that individuals with vein disease may be at increased risk for venous ulcers or deep vein thrombosis (DVT). Venous ulcers are open, non-healing wounds that are a sign of progressing vein disease. Deep vein thrombosis (DVT) is a serious type of blood clot that develops within the deep venous system.
DVT can place you at risk for a life-threatening condition called pulmonary embolism. This occurs when a piece of the clot breaks off and travels to the lung. Pulmonary embolism requires immediate emergency care.
Vein Disease Treatment
At USA Vein Clinics, our vein specialists offer a range of leading-edge, minimally invasive treatment options. Although each option varies in approach, they all have a similar goal: to close off blood flow to malfunctioning veins and divert it to healthy, surrounding ones.
Our vein disease treatment options include:
- Endovenous Laser Therapy (EVLT): EVLT uses ultrasound guidance to place a very thin laser fiber into the diseased vein. Then, laser energy is applied to seal it off.
- Visual sclerotherapy: This technique can be used on very small veins, such as spider veins. Your vein specialist inserts a tiny needle with a sclerosant (a type of irritant) into the affected vein, causing it to collapse.
- Varithena Vein Treatment: This treatment uses a type of medical foam to close off malfunctioning veins. When performing the procedure, your doctor will use ultrasound imaging for guidance.
- ClariVein®: ClariVein® involves the use of a rotating catheter along with the injection of a medical solution. These elements work together to close targeted veins and divert blood flow to healthy ones.
- Ultrasound-Guided Sclerotherapy – This nonsurgical treatment is used for veins that are close to the surface of the skin. Using ultrasound guidance, your vein specialist injects sclerosants intended to irritate and collapse targeted veins.
- VenaSeal™ Treatment: Our latest treatment option involves the use of a medical adhesive to seal varicose veins closed. Unlike other treatments, patients are not required to wear compression socks during recovery.
Request a Consultation at USA Vein Clinics
For personalized recommendations on how to improve your vein health, turn to the experts at USA Vein Clinics. Our experienced vein specialists provide non-surgical treatment for varicose veins, spider veins, and a range of venous conditions.
Our minimally invasive treatments are performed in state-of-the-art outpatient clinics across the nation. Most of them take less than an hour from start to finish, allowing you to leave immediately afterward and return to most normal activities.
To get started, schedule an appointment online or call 888.768.3467 today. You can choose to attend a virtual doctor consultation or visit us in person at one of our convenient clinic locations.
Vein Disease Frequently Asked Questions (FAQs)
1. What is Vein Disease?
Vein disease, also known as venous insufficiency, is the underlying cause of varicose veins, spider veins, and other venous issues. Vein disease occurs when veins are placed under strain due to a variety of factors. Chronic strain can lead to damaged vein valves, which are unable to pump blood efficiently back to your heart. This causes blood to pool in various areas of the body, which may lead to painful and uncomfortable symptoms. Most commonly, the legs, ankles, and feet are impacted.
If you have vein disease, you may experience a range of mild, moderate, or severe symptoms. Because vein disease is progressive, your symptoms may worsen over time.
Common symptoms of vein disease in legs include:
- Swelling in the legs and ankles
- Tired, aching legs
- Numbness or tingling sensations
- Difficulty standing for long periods
- Non-healing wounds on your legs
- Burning in the calf or thigh
- Leg pain that feels better when you walk or raise your legs
- Itchy, dry skin
If you are experiencing venous disease symptoms, consult a vein specialist.
2. What are Risk Factors for Vein Disease?
There are many potential reasons why people develop vein disease. Some are hereditary, whereas others can sometimes be controlled with healthy lifestyle choices. You may be at increased risk for venous disease if you are:
- A close relative of someone with vein disease
- Obese or overweight
- Female
- Over 50
- Pregnant
- In a job that requires prolonged standing or sitting
- Hypertensive (high blood pressure)
- Diabetic
If you are at increased risk for developing vein disease, close monitoring by a vein specialist may be beneficial.
3. Is Vein Disease Common?
Vein disease is a common health condition in the United States. As many as 17% of men and 40% of women may be impacted. Unfortunately, only a small fraction of those affected seek treatment.
4. How Can I Improve my Vein Health?
There are several things you can do to reduce your risk for vein disease and keep current venous symptoms from getting worse.
We generally recommend:
- Lose excess weight
- Eat a healthy, well-rounded diet
- Limit alcohol and caffeine
- Exercise regularly
- Don’t smoke
- Manage other health conditions like high blood pressure and diabetes
- Avoid standing or sitting for prolonged periods
- Ask your doctor about wearing compression socks
- Consider minimally invasive vein treatment
5. What Types of Vein Treatments are Available?
At USA Vein Clinics, we offer a range of minimally-invasive, office-based vein treatments. All of our methods aim to seal off the diseased vein(s). Blood flow is then diverted to healthy, surrounding veins.
Your vein specialist will help determine which method is best for you. Your vein disease treatment plan may include:
- Endovenous laser therapy (EVLT)
- ClariVein®
- Varithena foam treatment
- Ultrasound-guided sclerotherapy
- VenaSeal™ treatment
- Radiofrequency Abalation (RFA)
When it comes to paying for vein treatment, we have good news. Generally, most major health insurance plans cover vein treatment. Please contact us at 888.768.3467 to discuss your coverage details.
Schedule Anytime, Anywhere
Skip the wait times! Scheduling at your fingertips, 24/7. Minimally invasive non-surgical treatment for spider & varicose veins.
Schedule Online