

p data-path-to-node=”6,0″>If you have varicose veins, you may notice more than visible changes in your legs. Many people experience aching, heaviness, throbbing, burning, or swelling especially after sitting or standing for long periods. For some, the discomfort eases overnight; for others, it becomes a persistent interference with daily life.
If this sounds familiar, you’re not imagining it. Varicose vein pain is real, progressive, and a sign of an underlying medical condition. Fortunately, there are ways to feel better today while also planning for the long-term relief that only a specialist can provide.
Why Do Varicose Veins Cause Leg Pain?


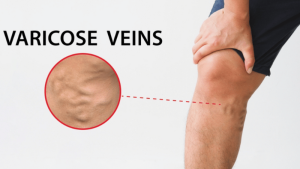
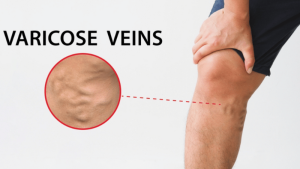
Varicose veins are enlarged, twisted leg veins that often appear blue or purplish beneath the skin. While many people think of them as a cosmetic issue, they are most often caused by chronic venous insufficiency (CVI) a medical condition that affects how blood flows through the legs.
Healthy veins contain one-way valves that move blood upward toward the heart. When these valves weaken or fail, blood flows backward and pools in the lower legs, a process known as venous reflux. Over time, this leads to:
- Stretching of vein walls, which reduces elasticity
- Inflammation of surrounding tissue, causing aching or burning sensations
- Increased venous pressure, often worse at the end of the day or in warm weather
These changes are what make varicose veins painful not just their appearance.
TAKE OUR QUIZ TO EVALUATE YOUR VEIN HEALTH
What Makes Varicose Vein Pain Worse?
Certain factors increase venous pressure and make symptoms more noticeable, including:
- Prolonged sitting or standing, which limits the calf muscles’ ability to pump blood upward
- Heat and dehydration, as heat dilates veins and dehydration thickens blood
- Weight gain, which increases physical strain on leg veins
- Pregnancy, due to hormonal changes and increased blood volume
- Travel, especially long flights or road trips with limited movement
If these triggers consistently worsen your symptoms, it may indicate that vein disease is progressing.
How to Relieve Varicose Vein Pain
Knowing what worsens varicose vein pain is important but it’s only part of the picture. Many patients want to know what they can do right now to reduce discomfort, especially when pain flares after a long day, travel, or prolonged standing.
There are two ways to relieve varicose vein pain: long-term and short-term.
Phase 1: Short-Term Varicose Vein Pain Relief (Conservative Therapy)


These at-home strategies focus on improving circulation and reducing pressure in the legs. They can help ease discomfort today, but they are considered conservative therapy, the first step many insurance providers require before approving medical treatment.
1. Elevate Your Legs
Raise your legs above heart level for about 15 minutes, two to three times a day. This allows gravity to help drain pooled blood from the lower extremities, reducing swelling and pressure.
2. Avoid Sitting or Standing for Too Long
Avoid standing for long and take movement breaks at least once every hour. Even a few minutes of walking or gently pedaling your feet while seated can activate the calf muscle pump.
3. Wear Loose Clothing and Supportive Shoes
Tight clothing around the waist or thighs can restrict circulation. Supportive, flat shoes allow the calf muscles to work more effectively.
4. Ease Discomfort With Hydrotherapy
Warm water can relax muscles, while finishing a shower with cool water on your legs may help veins constrict and reduce swelling.
5. Stay Hydrated
Proper hydration supports healthy blood viscosity. When blood flows more easily, there is less strain on already-damaged veins.
6. Wear Medical-Grade Compression Stockings
Compression stockings provide external support that helps veins move blood upward and can significantly reduce symptoms when properly fitted.
Note: Many insurance providers require documented use of compression stockings for a specific period before covering minimally invasive vein treatments.
As valve damage progresses, conservative therapy often becomes less effective. This is not a failure, it’s a sign that the underlying condition may need medical attention.
Phase 2: Long-Term Varicose Vein Pain Relief (Treating the Root Cause)


Lasting relief requires addressing the failed valves and pooling blood itself. These steps bridge the gap between managing symptoms and eliminating the source of pain.
7. Practice Daily Leg Stretches
Exercises such as calf raises and ankle circles strengthen the calf muscles often called the second heart and improve venous return.
8. Stay Active During Travel and Desk Work
Regular ankle flexing, leg stretches, and short walks help prevent blood from pooling during long periods of sitting.
9. Follow a Vein-Friendly, Anti-Inflammatory Diet
Reducing sodium helps limit swelling, while increasing fiber prevents strain. Foods rich in bioflavonoids, such as berries and leafy greens, support vein wall health.
10. Consult a Vein Specialist for Diagnostic Evaluation
The most effective way to relieve varicose vein pain is by treating the damaged veins themselves. A specialist can determine whether your symptoms are caused by progressive vein disease and recommend appropriate care.
When to See a Vein Doctor About Leg Pain


Short-term relief can help, but you should seek medical evaluation if you experience:
- Pain that interferes with sleep or daily activities
- Swelling that does not improve overnight
- Skin changes such as discoloration, itching, or thickening near the ankles
- Any non-healing sore or ulcer on the lower leg
How a Vein Ultrasound Identifies the Cause of Pain
At USA Vein Clinics, specialists use duplex ultrasound to visualize blood flow in real time. This diagnostic step is essential for:
- Identifying which vein valves have failed
- Establishing medical necessity for insurance coverage
- Creating a personalized treatment plan
Lasting Relief Through Minimally Invasive Treatment
When vein disease is confirmed, FDA-approved, in-office treatments can address the root cause. These procedures typically take about 30 minutes and do not require a hospital stay or general anesthesia.
Treatment options include:
-
Endovenous Laser Therapy (EVLT) and Radiofrequency Ablation (RFA), which use thermal energy to seal diseased veins
-
VenaSeal™, a medical adhesive that closes the vein instantly
-
Ultrasound-Guided Sclerotherapy, which treats veins that are twisted or not visible on the surface
Once treated, blood is naturally rerouted to healthy veins, and the damaged vein is gradually reabsorbed by the body.
Because these procedures treat chronic venous insufficiency, they are typically covered by most major insurance plans, including Medicare and Medicaid.
Discover Effective Varicose Vein Pain Relief at USA Vein Clinics
If your legs are telling you something is wrong, don’t wait for the pain to worsen. Most vein evaluations are covered by insurance, and no referral is required.
USA Vein Clinics has over 160 non-surgical vein treatment centers across the country, making high-quality vein treatments more accessible. Our services are typically covered by most major health insurance plans, including Medicare and Medicaid.
There’s no need to suffer from varicose vein pain any longer. If you’d like to learn more about how our treatments can provide varicose vein leg pain relief, please contact us. You can call (888) 768-3467 or schedule an appointment online.
Frequently Asked Questions
What does it mean when varicose veins hurt?
If your varicose veins hurt, it means your veins are stretched or inflamed, or that fluid build-up caused by damaged leg veins is causing swelling and inflammation.
What does varicose vein pain feel like?
Varicose vein pain is a deep, throbbing pain that feels better when you elevate your legs. You might also notice leg heaviness, calf cramps, and an overall sense of achiness in your legs and feet.
What is the best way to relieve varicose vein pain?
Treatment to target damaged veins is the most effective way to relieve painful varicose vein symptoms. Treatment addresses the root cause and can ease pain, swelling, and other uncomfortable symptoms while also reducing the appearance of leg veins.
STILL HAVE QUESTIONS? CALL US TODAY TO MAKE AN APPOINTMENT
References
- Joseph C Watso and William B Farquhar, “Hydration status and cardiovascular function,” Nutrients 11 no. 8 (2019): 1866.





