Experiencing a vein collapse might sound like an alarming medical event, but, in truth, vein collapse is common and treatable. Vein collapse results from damage to the vein walls, in which the veins cave inward, causing a blockage in blood flow. A range of underlying factors can cause it, including injury to the vein, repeated needle insertions, and medical conditions such as chronic venous insufficiency (CVI). CVI is also known as vein disease, with symptoms such as varicose and spider veins.
USA Vein Clinics can diagnose and treat vein-related issues, especially if caused by collapsed veins. Early treatment can resolve collapsed veins and prevent further complications. In this blog, we’ll look at what collapsed veins are, what causes them, when to be concerned, and how collapsed veins are treated.
What Is a Collapsed Vein?
When a vein collapses, it cannot carry blood back to the heart due to a loss of structural integrity. As a result, surrounding veins take on additional blood flow to compensate for the collapsed vein’s loss. This added pressure can weaken surrounding veins, increasing the likelihood of developing complications such as varicose veins.
Why Should You Be Concerned About a Collapsed Vein?
When veins collapse, it restricts blood flow, leading to discomfort and increasing the risk of serious medical complications. Common symptoms of restricted blood flow include pain, swelling, and tenderness in the affected area.
If left untreated, collapsed veins can contribute to more serious conditions, such as:
- Deep vein thrombosis (DVT): If the blood clot forms in a deep vein, it can lead to DVT, which can cause severe pain and swelling. In some cases, a blood clot can lead to vein collapse.
- Pulmonary embolism (PE): In some cases, the blood clot can break loose and travel to the lungs, causing a potentially life-threatening condition.
SCHEDULE AN APPOINTMENT ONLINE
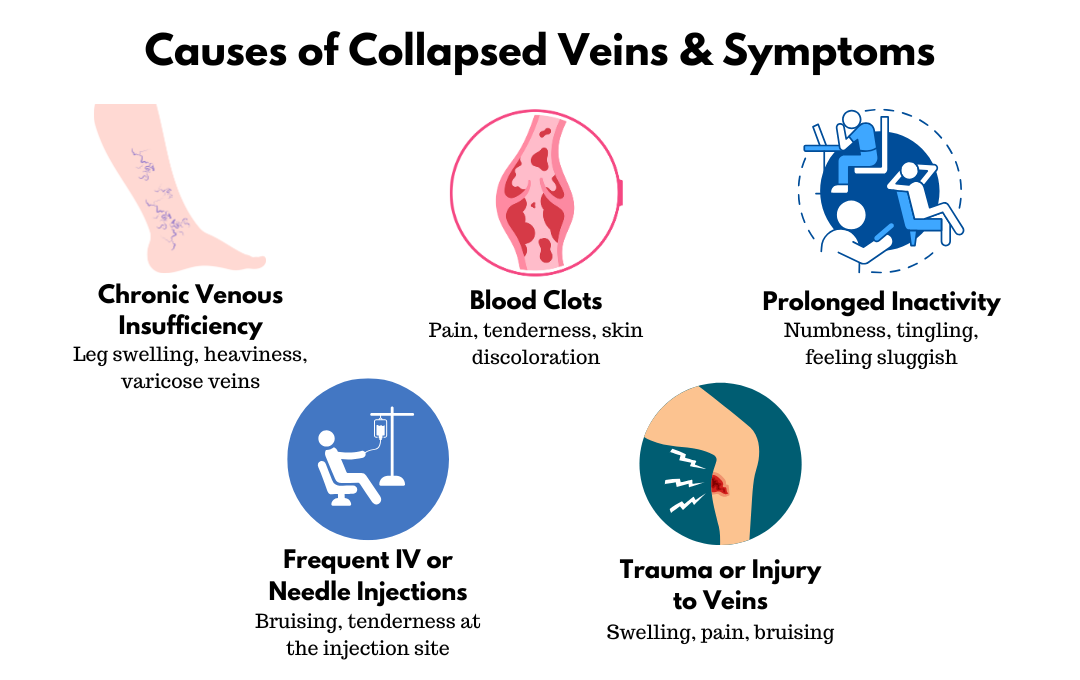
What Causes Veins to Collapse?
There are multiple underlying causes for vein collapse. Some of the most common causes include:
- Chronic venous insufficiency (CVI)
- Blood clots
- Prolonged inactivity
- Frequent IV or needle insertions in the same vein
- Aging
- Trauma or injury to veins
The causes of vein collapse can create extra pressure in the veins, making them swell. This can weaken the vein walls to the point that they start to collapse.
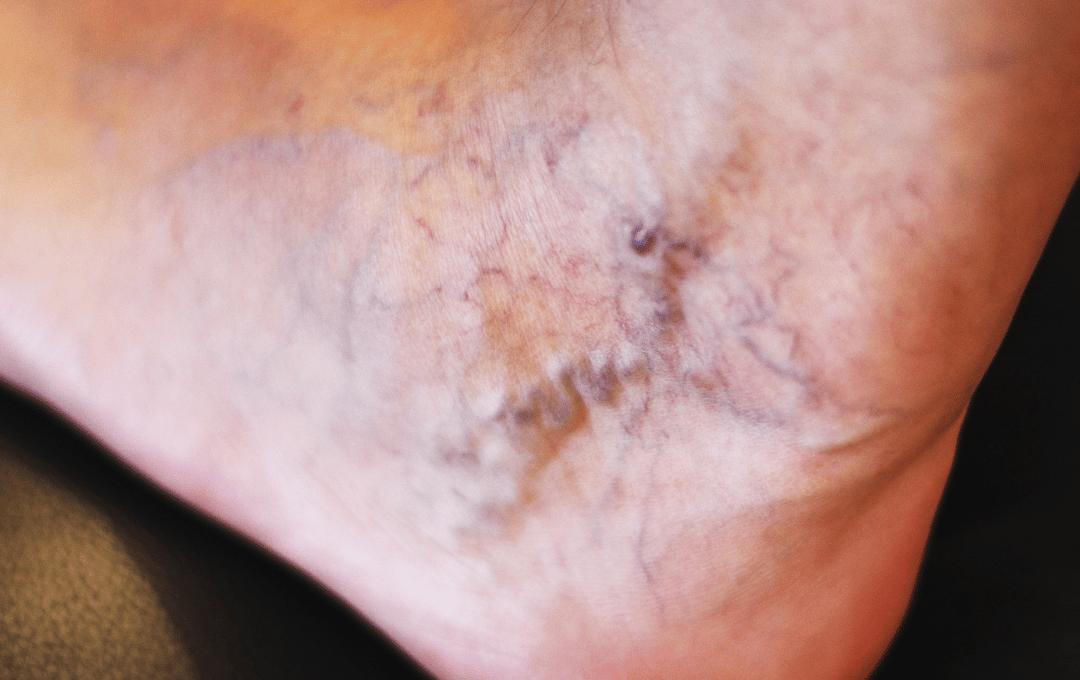
Recognizing What A Collapsed Vein Looks Like
Collapsed veins often cause noticeable symptoms, such as skin discoloration and bruising. Additional signs of collapsed veins include:
- Swelling around the vein
- Tenderness around the affected vein
- Difficulty having blood drawn
It may be difficult to see a collapsed vein underneath the skin. If you are experiencing additional symptoms of poor circulation, such as leg heaviness or dry, itchy skin, seek a consultation with a vein specialist to determine what’s causing your symptoms and what can be done to treat them.
If you’ve noticed any symptoms of collapsed veins, contact USA Vein Clinics for a proper diagnosis by calling 888.768.3467 or schedule online.
You can also take our free quiz to see if your symptoms may be related to vein issues.
Can Collapsed Veins Heal?
Collapsed veins can heal, but recovery time depends on factors such as the severity of the collapse and any underlying conditions. A vein specialist can explain the best treatment options for your situation and how long it will take to resolve the vein collapse.
Treating Collapsed Veins with Minimally Invasive Treatments
Minimally invasive treatments offered at USA Vein Clinics aim to restore blood flow by various methods. These methods can include using a solution, medical-grade adhesive, laser heat, or radiofrequency heat, which can be personalized to each patient’s needs. When the vein specialist administers treatment, the process will seal the veins shut, and the blood will naturally reroute to healthier veins. The collapsed vein will be reabsorbed into the body.
USA Vein Clinics has over 168 locations nationwide, providing convenient vein care to patients seeking relief from varicose veins and other vein issues. If you are curious about the vein treatments we offer, you can view them here.
Preventing Collapsed Veins
If chronic venous insufficiency is causing your veins to collapse, prevention tips for this condition may also help lower your risk of collapsing veins. This can include staying active, eating a balanced diet, and avoiding prolonged inactivity, which can help strengthen veins.
Regular vein screenings are among the most effective ways to detect potential issues early and prevent complications. USA Vein Clinics has nationwide locations and accepts most insurance plans. Our physicians can diagnose vein issues and provide minimally invasive treatments to improve circulation and relieve symptoms. Contact us today for a vein health appointment.
FAQS
Are collapsed veins permanent?
Collapsed veins do not repair themselves, but treatment can alleviate symptoms and improve circulation by rerouting blood flow.
Can dehydration contribute to vein collapse?
Dehydration thickens the blood, increasing the risk of clotting and putting added strain on veins. This can contribute to vein damage and collapse.
What is the difference between a blown vein and a collapsed vein?
A blown vein occurs when a needle or IV injection punctures through the vein and out the other side, leading to bruising, discoloration, and mild swelling around the injection site.
A collapsed vein happens when a vein caves inward, restricting blood flow. While blown veins usually recover, collapsed veins may not heal and need treatment.
Is a collapsed vein dangerous?
Collapsed veins aren’t life-threatening but do increase the risk of poor circulation. Poor circulation can lead to tissue damage. Additionally, collapsed veins increase your risk of severe blood clots.