Have you ever struggled with tired, heavy legs at the end of the day? Do you notice your ankles swelling after standing, or have you seen new spider veins appearing on your calves?
While it’s easy to dismiss these changes as “just getting older” or the result of a long work shift, they are often the warning signs of Chronic Venous Insufficiency (CVI).
CVI is a progressive medical condition, meaning it will get worse over time if left untreated. It affects nearly 40% of the U.S. population, yet many people live with the discomfort unnecessarily.
The good news? CVI is highly treatable. Recognizing the stages early is the key to preventing permanent skin damage, avoiding Deep Vein Thrombosis (DVT), and restoring your quality of life.
Request a Vein Consultation Today
What is Chronic Venous Insufficiency (CVI)?
To understand why your legs hurt, you have to understand how your veins work.
Your arteries pump oxygen-rich blood from your heart to your extremities. Your veins have the difficult job of pushing that blood back up to the heart, fighting gravity the entire way. To do this, your leg veins rely on tiny, one-way valves.
The Root Cause: When these valves become damaged or weak (due to age, genetics, or pressure), they cannot close properly. Blood leaks backward and pools in the lower legs. This condition is called venous reflux. As the blood pools, the pressure inside the veins skyrockets (venous hypertension), causing the veins to stretch, bulge, and leak fluid into the surrounding tissue.
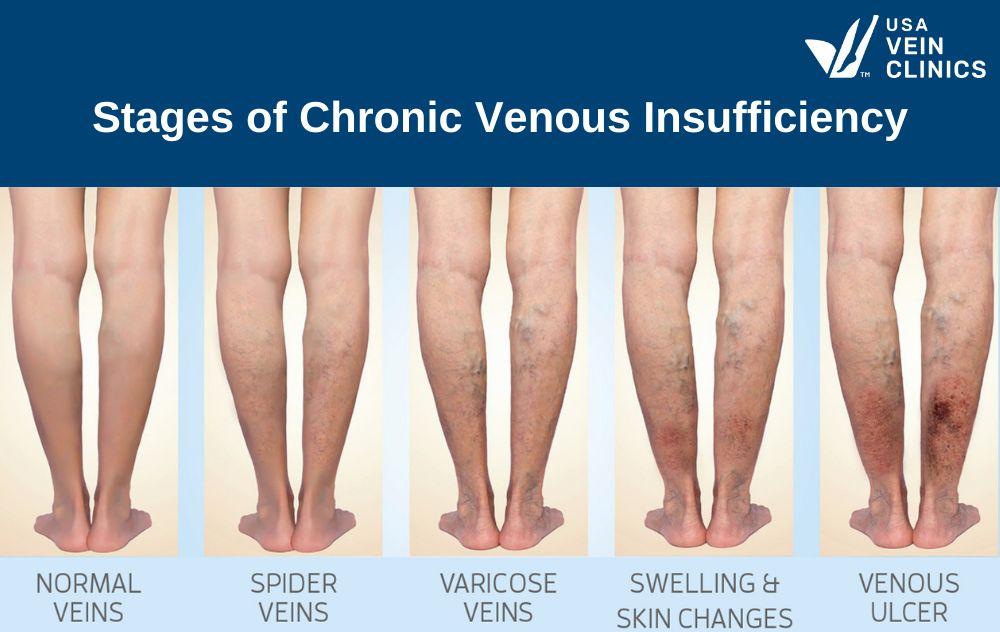
This progression is categorized into 6 distinct stages, known medically as the CEAP classification.
The 6 Stages of Vein Disease (CEAP Guide)
Doctors use the CEAP scale to evaluate the severity of vein disease. Identifying where you fall on this scale is the first step toward getting insurance coverage for your treatment.
Stage 1: Spider Veins & Reticular Veins
- Visual Signs: You will see tiny, web-like veins on the skin’s surface. They can be red, blue, or purple. You might also see reticular veins (sometimes called “feeder veins”), which are slightly larger blue veins that do not bulge.
- Physical Symptoms: While often painless, many patients report a burning sensation, itching, or minor throbbing around the clusters of veins.
- The Verdict: Early Warning. Your circulation is struggling. While Stage 1 is often considered cosmetic by insurance providers, it is a signal that your valves are beginning to fail.
- Action: A vein screening now can rule out deeper issues before they become visible varicose veins.
Stage 2: Varicose Veins
- Visual Signs: These are the most recognizable signs of CVI. Varicose veins are enlarged, rope-like veins that bulge above the skin’s surface. They may appear twisted, knotty, or dark purple.
- Physical Symptoms: This is where physical discomfort usually becomes daily. You may experience:
- Heaviness: Legs feel like lead weights by the afternoon.
- Pain: Throbbing, aching, or cramping (especially “charley horses” at night).
- Restless Legs: An uncontrollable urge to move your legs when trying to sleep.
- The Verdict: Medical Necessity. The structural damage to your veins is significant. Most insurance plans cover treatment at this stage because varicose veins can lead to blood clots if ignored.
Stage 3: Leg Swelling (Edema)
- Visual Signs: Your ankles or calves look puffy or swollen. You may notice “pitting edema”, where pressing a finger into your ankle leaves a dent that takes a few seconds to disappear.
- Physical Symptoms: Your shoes may feel tight by the end of the day, or your socks may leave deep indentation marks on your shins. The swelling often goes down after sleeping with legs elevated but returns the next day.
- The Verdict: Progressive Damage. The pressure in your veins is now high enough that fluid is leaking out of the vein walls and into the surrounding tissue. This chronic swelling can damage your lymphatic system over time.
Stage 4: Skin Changes (The Danger Zone)
At this stage, the chronic inflammation begins to damage the skin and soft tissue. This is often split into two sub-stages:
- 4A (Pigmentation/Eczema): You may develop Stasis Dermatitis, a red, itchy rash often mistaken for eczema. You might also see brown or rusty discoloration (Hemosiderin staining) caused by iron from red blood cells leaking into the skin.
- 4B (Lipodermatosclerosis): The skin becomes hard, thick, and leathery. The lower leg may look tapered, resembling an upside-down champagne bottle.
- The Verdict: Advanced Disease. Your skin is becoming fragile. The blood supply to the skin is compromised, placing you at high risk for open wounds.
Stage 5: Healed Venous Ulcers
- Visual Signs: You have a scar or discolored area from a sore on your leg or ankle that previously opened and has since healed.
- The Verdict: High Recurrence Risk. A healed wound does not mean the vein is fixed. The underlying high pressure (venous hypertension) is still there. Without closing the diseased vein, the ulcer is highly likely to open again.
Stage 6: Active Venous Ulcers
- Visual Signs: Open, weeping wounds, usually located on the inside of the ankle or lower leg. These sores are often shallow with irregular borders and a red base.
- Physical Symptoms: These ulcers can be extremely painful and tender. They resist standard healing methods (like creams or bandages) because the high vein pressure prevents fresh oxygen from reaching the tissue.
- The Verdict: Medical Emergency. Open ulcers carry a high risk of serious skin infections (cellulitis). Immediate intervention is required to heal the wound and treat the underlying vein disease.
Do You Recognize These Symptoms? You don’t have to live with leg pain, hiding your legs, or worrying about ulcers. Modern vein treatments are minimally invasive, require no downtime, and are covered by most insurance plans (Stages 2–6).
How is Chronic Venous Insufficiency Diagnosed?
If you suspect you have CVI, a visual check isn’t enough. At USA Vein Clinics, we utilize advanced diagnostic tools to see inside your legs.
Duplex Ultrasound Scan: This is the gold standard for vein diagnosis. It is a painless, non-invasive test that uses sound waves to create a map of your veins. It allows the doctor to:
- Measure the speed and direction of blood flow.
- Identify exactly which valves have failed.
- Check for any deep vein blood clots (DVT).
This detailed vein map allows us to customize a treatment plan that targets the root of the problem, not just the surface symptoms.
Common Risk Factors: Are You at Risk?
While anyone can develop CVI, certain factors increase your likelihood of valve failure:
- Genetics (The #1 Factor): If your parents had varicose veins, your risk increases to over 80%.
- Pregnancy: Increased blood volume and pressure on the pelvis strain leg veins. Multiple pregnancies increase the risk.
- Occupation: Jobs that require prolonged standing (nurses, teachers, servers) or sitting (drivers, office workers) prevent the calf muscles from pumping blood efficiently.
- Age: As we age, vein walls naturally lose elasticity, causing them to stretch and valves to separate.
- Obesity: Excess weight puts added pressure on the leg veins, accelerating valve damage.
Treatment Options: Non-Surgical & Minimally Invasive
Gone are the days of painful “vein stripping” and hospital stays. Modern vein treatment is performed in our office, takes less than an hour, and allows you to walk out immediately.
- Endovenous Laser Therapy (EVLT): We insert a thin fiber into the diseased vein using ultrasound guidance. Laser energy is used to heat and seal the vein shut. Your body naturally reroutes blood to healthy veins, and the symptoms resolve.
- Radiofrequency Ablation (RFA): Similar to EVLT, this uses radiofrequency energy to gently heat and collapse the damaged vein wall. It is the preferred method for treating large varicose veins.
- Ultrasound-Guided Sclerotherapy: For winding or twisted veins that are difficult to reach with a laser, we inject a specialized medical foam. This foam irritates the vein lining, causing it to seal closed. This is often used for Stage 1 spider veins or smaller varicose tributaries.
Why You Shouldn’t “Wait and See”
A common misconception is that varicose veins are just a cosmetic annoyance. This is false.
Ignoring CVI in the early stages (1–3) often leads to the advanced complications of stages 4–6. Furthermore, untreated CVI is a leading risk factor for Deep Vein Thrombosis (DVT). DVT is a serious blood clot in the deep veins that can break loose and travel to the lungs, causing a potentially life-threatening Pulmonary Embolism.
Take the Next Step for Your Health
Don’t wait for skin changes or ulcers to appear. The earlier you treat CVI, the easier the recovery.
At USA Vein Clinics, our specialists are ready to diagnose your specific stage of CVI and create a personalized plan to restore your circulation and confidence.
Request a Vein Consultation Today
Chronic Venous Insufficiency FAQs
What Are the Visible Signs of CVI?
Venous insufficiency has different stages so that you might notice certain visible signs at each stage.
- In the early stages, you’ll see visible veins, including spider veins and varicose veins. You also might notice leg swelling.
- As it advances, you’ll see skin changes, including hardened, waxy-looking skin, red rashes, and skin wounds that heal slowly or don’t heal at all.
What Does Venous Insufficiency Look Like?
Venous insufficiency manifests in various stages, each characterized by distinct visible signs. In the early stages, individuals may notice the appearance of spider veins or varicose veins, which are visible beneath the skin’s surface. These veins may present as tiny, colorful, web-like patterns (spider veins) or enlarged, twisted veins that protrude above the skin’s surface (varicose veins). Additionally, leg swelling may occur, particularly as the condition progresses.
As venous insufficiency advances, changes in the skin become more apparent. This may include the development of hardened, waxy-looking skin, red rashes (venous stasis dermatitis), and skin wounds that heal slowly or not at all. These visible signs indicate worsening vein health and should prompt individuals to seek evaluation and treatment from a vein specialist.
During Which Chronic Venous Insufficiency Stage Should You Get Treatment?
If you notice any signs of chronic venous insufficiency, it’s important to see a vein specialist. An experienced doctor can examine your symptoms and determine the stage. They will also provide a personalized treatment plan that can help restore your vein health.
USA Vein Clinics is a nationwide clinic staffed with experienced vein doctors. We can diagnose and treat your veins, no matter what stage of venous insufficiency you’re experiencing, helping to relieve your symptoms, support better circulation, and improve your overall vein health.
What Happens if Chronic Venous Insufficiency Is Left Untreated?
CVI is a progressive disease that will continue to get worse. If you have signs of early venous insufficiency, such as spider veins or varicose veins, you should see a vein specialist. Varicose veins don’t have a cure, but they are treatable.
If ignored, chronic venous insufficiency (CVI) can lead to severe complications, including deep vein thrombosis (DVT) and potentially even leg amputation. DVT is when a blood clot forms within a deep vein, usually in the legs. If left untreated, these clots can break loose and travel through the bloodstream, potentially causing a pulmonary embolism if they reach the lungs, which can be life-threatening. Additionally, untreated CVI can result in the development of venous ulcers, persistent wounds on the legs that are challenging to heal and increase the risk of serious skin infections.
There’s also the pain, swelling, and daily discomfort of the symptoms that typically appear in the more advanced stages of chronic venous insufficiency.
References:
Patel SK, Surowiec SM. Venous Insufficiency. [Updated 2023 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430975/