Topics Covered:
- Varicose Vein Basics
- Anatomy of a Blood Clot
- Link Between Varicose Veins and Blood Clots
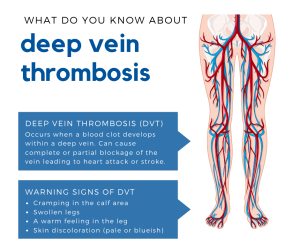
- Warning Signs of Blood Clots in the Legs
- Managing Varicose Veins and Clot Risks
Varicose veins are swollen, twisted blood vessels that bulge just under the skin’s surface. Although varicose veins may be unsightly and uncomfortable, they are not typically considered a direct indicator of dangerous blood clots, such as deep vein thrombosis (DVT).
However, the symptoms of varicose veins can be similar to those of blood clots. Understanding the differences between these conditions is important to recognize the warning signs of a potentially fatal blood clot.
If left untreated, they can lead to an increased risk of blood clots in the form of superficial venous thrombosis (SVT) or, in some cases, deep vein thrombosis. Deep vein thrombosis (DVT) is a life-threatening emergency that requires urgent medical attention.
This article will help you learn the signs, symptoms and connection between varicose veins and blood clots.
Varicose Veins: The Basics
Varicose veins can appear as bulging, twisted, discolored blood vessels near the surface of the skin in the legs, feet or ankles. While not everyone with varicose veins has noticeable symptoms, those who do may experience the following:
- Swelling in the legs, ankles, or feet
- Ulcerations or open wounds on the skin
- Rough, scaly, or hardened skin
- Tiredness or heaviness in the legs
- Cramping and achiness in the calf or thigh
- Leg pain that is alleviated by walking or elevation
- Itchy or burning sensations around the affected veins
- Restless legs while sleeping
In a healthy state, veins use one-way valves to keep blood flowing upward and prevent backflow. Over time, disease and damage can impair the elasticity of the vein walls, causing the valves to malfunction, a condition called venous insufficiency. With nothing to stop the backflow, blood follows gravity into the veins of the lower extremities, where it begins to pool. The excess blood exerts pressure on the vein walls making them weak, and eventually leading to the formation of varicose veins and spider veins.
Worried about your vein health?
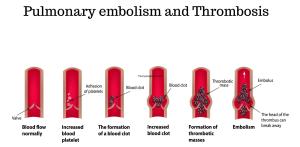
Anatomy Of a Blood Clot

A blood clot is a gel-like, semi solid clump of blood cells resulting from blood coagulation in the blood vessels and veins. When a blood clot forms, the skin around the area experiences redness and swelling. This may occur due to an external or internal injury.
When these blood clots develop, they may travel to other parts of the body creating a blockage and congestion. Some blood clots are hard to identify as they present little or no symptoms. However, it is crucial to look out for common signs and symptoms of blood clots such as swelling, leg pain, varicose veins, red and tender skin to avoid serious conditions like DVT.
The Link Between Varicose Veins and Blood Clots
If you have varicose veins, you might be at higher risk of developing a blood clot. Diseases of the circulatory system can be isolated events, but can also be interconnected to other disease processes. Venous insufficiency is a risk factor for developing a thrombus — a blood clot that forms inside a blood vessel.
Your blood is made up of many components, including water, red and white blood cells, platelets, sugars, and proteins. These components work together to deliver oxygen and essential nutrients to tissues and organs throughout your body.
When arteries and veins are damaged, the flow of blood gets disrupted. Damage results in inflammation at the cellular level, causing the blood vessels to narrow out and restrict blood flow and blood to bind inside of the vessel walls.
The components of blood can be thought of as a little sticky. When blood is moving quickly, the red blood cells slide past each other with very little friction. But when blood flow becomes compromised, blood moves more slowly, increasing the risk of its components sticking together to form a clot. Blood clots in the veins are known as venous thromboembolism (VTE), a term that encompasses both DVT and pulmonary embolism.
Varicose veins develop in the veins close to the surface of the skin. Affected veins usually appear large, twisted, discolored, and bulging. While venous thromboembolism generally occurs in the deep veins (the veins below the muscle), research has shown that individuals who suffer from varicose veins are more likely to develop a blood clot.
Venous thromboembolism can cause two types of blood clots: superficial venous thrombosis (SVT) and deep vein thrombosis (DVT).
Venous problems won’t disappear on their own. Take charge of your health now.
Superficial Venous Thrombosis (SVT)
Superficial veins are those close to the skin. A blood clot that forms in the superficial blood vessels is called superficial venous thrombosis or superficial thrombophlebitis.
SVT is generally less serious than DVT, but it can progress to deep vein thrombosis if the clot increases in size and extends to a deeper vein. If you have an SVT, you may feel a swollen, tender feeling in the affected vein.
While varicose veins do not directly cause SVT, they may increase your risk of developing the condition by disrupting blood flow and causing inflammation.
Understanding Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a type of blood clot that occurs deep in the veins of the leg, thigh or pelvis, right beneath the muscle, running close to the bones of the lower extremities.
Under normal conditions, blood is in a liquid state. When a thrombus forms, blood cells clump together with platelets and proteins in the blood and form a solid mass in the veins.
A clot can partially or completely block blood flow in that vein. However, if the thrombus or a piece of it becomes dislodged, it can travel back to the heart and lungs. When the clot reaches the pulmonary artery (the artery that carries blood from your heart to your lungs) or one of its branches, it can become stuck, preventing your blood from releasing waste and receiving the oxygen it needs. This is referred to as a pulmonary embolism, or PE.
A DVT or PE can be life-threatening and should be evaluated by emergency services right away.
Recognizing Warning Signs
It can be hard to distinguish pain generated from varicose veins and that from a blood clot. The symptoms of a DVT are usually only felt in the limbs affected by the clot, but can also occur in both legs. Symptoms and signs of DVT to be aware of include:
- Swelling in the leg
- Pain in the legs, ankles, or feet
- Tenderness at the spot or around the clot
- Warm skin, especially compared to the other leg
- Redness or discoloration
Pulmonary embolism on the other hand causes additional symptoms, such as:
- Chest pain
- Shortness of breath
- Coughing
- Dizziness
- Heart palpitations (racing heartbeat)
If you experience any of these symptoms, seek urgent medical attention.
Managing Varicose Veins and Clot Risks
Your risk of developing varicose veins or blood clots depends on many factors. Some of these factors are genetic, but some are determined by lifestyle choices.
Varicose vein risk factors include:
- Family history of varicose veins
- 50 years of age or older (although venous issues can occur at any age)
- Being female (although males can develop them as well)
- Being overweight or obese
- Inactivity/lack of exercise
- Long periods of standing or sitting
- Underlying conditions like high blood pressure and diabetes
DVT risk factors include:
- Personal or family history of DVT
- 50 years of age or older (although venous issues can occur at any age)
- Trauma (for example, a recent surgery or injury)
- Varicose veins
- Alcohol
- Smoking
- Cardiovascular disease
- Long periods of sitting or standing
You cannot control if you are genetically predisposed to developing a blood clot or varicose veins, but you can control lifestyle choices that may increase your risk. If you’re concerned about developing varicose veins and blood clots, incorporating these proactive steps into your daily life can help mitigate your risk:
- Regular exercise
- Change leg positioning regularly, even while sitting
- Managing your weight
- Avoid smoking
- Elevating your legs with a pillow while resting
Talking to a Vein Specialist
Don’t let varicose veins develop into something far more serious. Venous insufficiency, varicose veins, and VTE don’t go away on their own and require appropriate treatment. We want you to know that help is available to alleviate the symptoms of these vein conditions.
If you carry risk factors for varicose veins or DVT, consult a medical professional as soon as possible. A vein specialist can help explore your personal risk factors and use imaging techniques to assess your vein health.
Schedule a Consultation with USA Vein Clinics
USA Vein Clinics has decades of experience treating complications of venous insufficiency. Varicose veins and spider veins can be treated with minimally invasive procedures at one of our outpatient clinics.
Take the first step in treating your leg vein problems and schedule a consultation at one of our many state-of-the-art clinics across the country. Our vein specialists will help diagnose your vein problems using the most current technology and offer you non-surgical solutions covered by most insurance carriers.
We know dealing with vein problems can be stressful. Our compassionate team will be by your side every step of the way.
Click here to start your journey to recovery today!