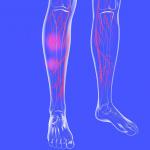
After a long day on your feet, your legs might feel heavy, achy, or slightly swollen. These sensations may seem harmless, but they can be early signs of blood pooling in the feet and legs. Blood pools when it collects in areas such as the legs and feet instead of circulating back to the heart. Over time, this pooling can cause discomfort, visible veins, or even skin changes.
Blood pooling is often linked to an underlying condition called chronic venous insufficiency (CVI). With CVI, vein valves weaken and struggle to push blood upward towards the heart, causing blood to stay in the legs and feet. Stagnant blood increases pressure in the lower extremities, leading to swelling, heaviness, and skin discoloration.
Learning to recognize early warning signs of blood pooling in the legs and feet is key to preventing progression and maintaining healthy circulation.
What is Blood Pooling?
Blood pooling is when the blood collects in your legs, feet, or ankle veins instead of returning to the heart. Typically, tiny one-way valves in your veins open and close to keep blood moving upward against gravity. When these valves become weak or damaged, blood can backflow and accumulate in the lower body.
Common symptoms of blood pooling in the legs include:
- Swelling
- Cramps
- Pain or soreness
- Skin discoloration
- Leg ulcers
- Varicose veins
This issue most often affects the legs, feet, and ankles because they’re the farthest from the heart and must work the hardest to push blood upward. While mild swelling after prolonged standing can be temporary, persistent blood pooling is not normal and typically requires medical attention.
What Does Blood Pooling in the Legs Feel Like?
Blood pooling, medically known as venous stasis, feels different for everyone, but most people describe a set of distinct, worsening sensations throughout the day. If you are experiencing blood pooling symptoms, you might recognize these specific feelings:
- “Leaden” Heaviness: Your legs may feel like they weigh twice as much as they should. This heavy leg sensation often makes it feel as if you are dragging your feet or walking through deep water, especially in the late afternoon.
- Deep, Dull Throbbing: Rather than a sharp pain, blood pooling often causes a rhythmic, pulsing ache. It feels as though the blood is stuck and pressing against the walls of your veins.
- Stretched or Taut Skin: As blood accumulates, swelling (edema) can make the skin on your shins and ankles feel “full” or stretched, as if it were a size too small for your legs.
- The Internal Itch: Many patients report an irritating, restless itch that feels deep beneath the skin rather than on the surface. A pins-and-needles or tingling sensation often accompanies this.
- Restless Hot Sensation: Your legs may feel warm to the touch, or you may experience an internal burning sensation that makes it challenging to keep them still at night.
If these sensations ease when you elevate your legs above your heart but return shortly after you stand, it is a classic indicator of chronic venous insufficiency.
What Conditions Are Linked to Blood Pooling?
Various factors can increase the likelihood of blood pooling in the legs, including obesity, pregnancy, and genetics. However, several underlying conditions can cause or worsen it, including:
- Chronic Venous Insufficiency (CVI): The most common cause of blood pooling, where vein valves become weak or damaged, causing blood to flow backwards and collect in the lower limbs.
- Venous Stasis Dermatitis: This condition develops from long-term blood pooling and poor circulation. The trapped blood and fluid leak into surrounding tissues, causing redness, itching, and scaling of the skin around the ankles or lower legs. The cause of venous stasis dermatitis is often chronic venous insufficiency (CVI).
- Lymphedema and Other Circulatory Disorders: Pooling of blood may also occur alongside lymphedema, in which lymph fluid builds up in the tissues, causing swelling and heaviness. Other circulatory disorders that impair fluid movement can similarly lead to increased pooling of the blood.
What Does Blood Pooling Look Like?
Blood pooling can cause visible changes in your legs, whether it’s swelling or bulging veins. Swelling is common around the ankles or calves, particularly after prolonged periods of sitting or standing. The skin may also show discoloration, turning red, brown, or even bluish as blood and fluid collect under the surface.
Is Blood Pooling Dangerous?
While occasional swelling or heaviness in the legs might seem harmless, chronic pooling of the blood can become dangerous if left untreated. Poor circulation increases venous pressure, leading to persistent swelling, skin breakdown, and painful leg ulcers. Persistent or worsening symptoms may signal underlying conditions such as chronic venous insufficiency (CVI).
In severe cases, stagnant blood flow can contribute to the formation of blood clots, including deep vein thrombosis (DVT), a potentially life-threatening condition. The most effective way to prevent these complications is to identify and address any early signs of pooling blood in the legs.
How Blood Pooling Is Diagnosed and Treated
Diagnosing the cause of blood pooling typically begins with a physical examination and may involve a duplex ultrasound to assess the blood flow in your veins. If vein-related issues, such as CVI or varicose veins, are detected, personalized treatment is recommended.
Patients can receive non-surgical vein treatments at USA Vein Clinics, performed in an outpatient setting with minimal downtime.
USA Vein Clinics offers treatments such as:
- VenaSeal™: Closes varicose veins with a medical adhesive.
- ClariVein®: Combines mechanical and chemical ablation to close varicose veins.
- Endovenous laser vein treatment (ELVT): Uses a laser fiber to seal damaged veins and redirect blood flow to healthier veins.
- Varithena® vein treatment: Involves injecting a foam sclerosant into the damaged vein to seal it shut.
- Ultrasound-guided sclerotherapy: An ultrasound is used to inject a sclerosant into the vein so it collapses damaged veins and redirects blood flow.
- Radiofrequency ablation (RFA): A catheter is inserted into the vein, and radiofrequency energy heats the vein to close it.
These treatments help restore healthy blood flow and alleviate symptoms such as swelling and heaviness, with minimal side effects. They also have a lower risk of complications than surgical procedures because they are minimally invasive.
How to Prevent and Manage Blood Pooling
While awaiting treatment, you can manage blood pooling in your legs with simple measures to relieve pressure on your veins.
These methods include:
- Elevating your legs above heart level for 15–20 minutes a few times a day
- Avoiding long periods of sitting or standing
- Focusing on exercises like walking, cycling, or calf stretches
- Wearing compression socks
- Drinking water and staying hydrated
- Maintaining a healthy weight
These lifestyle changes can temporarily ease discomfort, but if blood pooling symptoms worsen, consult a vein specialist for an evaluation.
When to See a Specialist for Blood Pooling at USA Vein Clinics
If you’re noticing persistent swelling, visible veins, leg discomfort, or skin changes, it’s time to seek expert evaluation. USA Vein Clinics’ focus is on diagnosing and treating symptoms, such as blood pooling, that indicate vein disease. Our minimally invasive treatments, such as endovenous laser vein treatment (EVLT), or ultrasound-guided sclerotherapy, are fast, require little downtime, and resolve painful symptoms that can interfere with your quality of life.
Additionally, USA Vein Clinics is recognized by the Intersocietal Accreditation Commission for Vascular Testing (IAC). This is the gold standard of vascular care, highlighting the clinics’ long-term commitment to providing the highest quality imaging and diagnostic standards for patient safety and accurate diagnosis across our 160+ nationwide locations.
Schedule a consultation today to determine whether you’re dealing with blood pooling caused by CVI.
FAQs About Blood Pooling
Can dehydration make blood pooling worse?
Dehydration can worsen blood pooling by thickening blood and reducing blood volume. These conditions can increase the risk of varicose veins, spider veins, and other circulatory issues.
Is blood pooling a symptom of heart failure?
Blood pooling is not necessarily a symptom of heart failure, as swollen lower extremities due to heart failure are due to fluid retention, known as edema. Pooling of the blood is a more common symptom of chronic venous insufficiency (CVI).
Is blood pooling the same as a blood clot?
Blood pooling and blood clots are not the same: blood clots are gel-like, semi-solid clumps of blood cells formed by coagulation in blood vessels and veins. Blood will pool when it is unable to return to your heart, causing it to collect in your legs, ankles, or feet.
Medically Reviewed By:
Dr. Yan Katsnelson is a philanthropist, business owner, and highly skilled cardiac surgeon. He is the Founder and CEO of USA Vein Clinics, which is part of USA Clinics Group, the parent company of USA Fibroid Centers, USA Vascular Centers, and USA Oncology Centers, with more than 160 facilities nationwide. Dr. Yan has established himself as a strong advocate for accessibility and affordability of the most advanced medical care close to home. His mission is to create a positive experience for each patient with compassionate, personalized, and expert care.