Vein disease can cause many symptoms and increase the risk of severe conditions, such as blood clots in the deep veins of the legs and ankles, known as deep vein thrombosis (DVT).
A blood clot in the ankle is easy to miss, as it can be mistaken for minor swelling or soreness while going about your day. However, along with pain and swelling, DVT also causes localized warmth and skin discoloration that doesn’t improve.
If left untreated, DVT, a part of the clot, can break off and travel through the bloodstream to the lungs, leading to pulmonary embolism (PE), a potentially life-threatening complication.
Identifying when ankle swelling or pain may signal a blood clot is vital for preventing severe complications and helping you seek timely treatment.
What Does a Blood Clot in the Ankle Feel Like?
Although it may not initially feel like something is wrong, a blood clot in the ankle can feel different from routine aches or soreness. Many patients describe an ankle blood clot as:
- Dull pressure or heaviness in the ankle
- Deep, throbbing pain, similar to a sprain or pulled muscle
- Warmth or heat around the affected area
Some people may not notice symptoms of a blood clot, making it even more important to identify potential causes of an ankle blood clot, such as vein disease.
Vein disease, also known as chronic venous insufficiency (CVI), occurs when the valves in the ankle veins are weakened or damaged, allowing blood to pool rather than flow back to the heart.
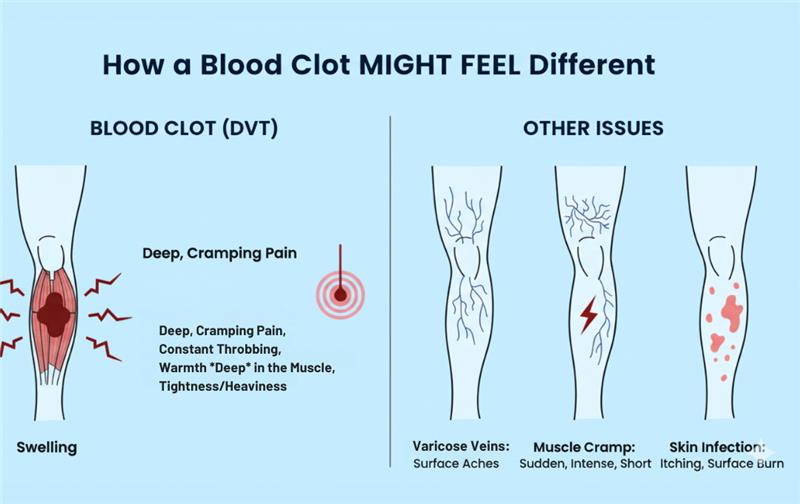
The Difference Between Pain Caused by Blood Clots and Muscular Ankle Pain
A blood clot in the ankle differs from other types of pain, such as muscle strain or joint pain, because it doesn’t follow a typical healing timeline.
Pain from deep vein thrombosis (DVT) in the lower leg or ankle often lingers and intensifies rather than resolving on its own, and isn’t typically caused by physical activity. With regular ankle pain, it usually results from physical activity and improves with rest, elevation, or ice.
What Are the Signs of a Blood Clot in the Ankle?
General swelling or pain, often caused by issues such as heart or kidney problems, tends to affect both ankles, while blood clots typically cause symptoms on one side of the body.
Along with feeling pain and tenderness, some common symptoms of a blood clot in the ankle include:
- Swelling that doesn’t improve overnight
- Skin discoloration, such as redness or a bluish tint
- Cramping or persistent soreness
Common Blood Clot in the Ankle Symptoms
Knowing the earliest stages, a blood clot in the ankle may cause more subtle symptoms, such as:
- Mild swelling in one ankle.
- Warmth or redness that doesn’t fade.
- Tightness or heaviness in the ankle.
- Discomfort while flexing the ankle or walking.
You can have a blood clot in your ankle without realizing it, as some blood clots don’t cause symptoms. Even then, early signs of blood clots in the ankle may seem less severe. However, they can progress rapidly, which is why understanding your risk level of blood clot formation and getting an early evaluation is critical.
One Swollen Ankle, No Pain: Is It a Blood Clot?
Having one ankle swollen, even without pain, can still be a sign of a blood clot. While swelling could stem from chronic venous insufficiency (CVI) or injury, it is important to rule out DVT as the cause first, as it carries a greater risk of pulmonary embolism (PE) and long-term vein damage.
Why Your Ankle Swells When a Clot Forms
A blood clot in the ankle can cause swelling by disrupting normal circulation. This disruption blocks blood flow, causing pressure to build in the veins and leading to fluid leaking into nearby tissues, which results in swelling.
Compared to typical fluid retention or injury swelling, clot-related swelling typically feels firmer, and veins may become more visible due to the increased pressure.
How Blood Clots and Vein Disease Are Connected
Vein disease can increase the risk of ankle venous blood clots. That’s because the weakened, damaged valves caused by varicose veins can impact healthy blood flow by causing it to pool or stagnate instead of pushing it back to the heart. This thickened blood can lead to the development of a clot. An ankle blood clot can also be a sign of deeper vein issues, such as:
- DVT (Deep Vein Thrombosis): A clot in the deep veins of the leg that causes pain, swelling, and discoloration
- CVI (Chronic Venous Insufficiency): When weakened vein valves cause blood to pool, increasing the risk of clotting and long-term swelling
Both conditions can coexist, as patients with a history of DVT are more likely to develop CVI, and chronic CVI increases the likelihood of future clot formation.
Risks of Untreated Blood Clots
Untreated blood clots in the ankle can cause both immediate and long-term complications.
These include:
- Pulmonary Embolism (PE): Occurs when a clot breaks free and travels to the lungs, blocking blood flow. This is an immediate, life-threatening medical emergency in which you need to seek medical help. Warning signs include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy
- Fainting
- Rapid pulse
- Rapid breathing
- Coughing up blood
- Chronic Venous Insufficiency (CVI): Long-term vein damage that causes persistent swelling, skin changes, and poor circulation.
An early diagnosis of DVT is vital. Timely treatment of vein disease using minimally invasive vein procedures can prevent severe complications.
Contact USA Vein Clinics Today
If you suspect blood clots or have symptoms of vein disease, USA Vein Clinics can provide a fast diagnosis using advanced imaging technology. Our nationwide clinics offer effective, minimally invasive vein treatments with little or no downtime.
Don’t ignore the signs of blood clots in your ankle. Schedule a consultation at USA Vein Clinics today and get expert care from America’s leading vein specialists.
FAQs About Blood Clots in the Ankle
How are blood clots in the ankle diagnosed?
A blood clot in the ankle is typically diagnosed through physical examinations and imaging tests, such as a duplex ultrasound. A duplex ultrasound uses sound waves to visualize blood flow and identify any blockages. Along with these tests, vein specialists will also check for symptoms such as pain, swelling, warmth, and redness. They also review your medical history and look for potential risk factors, such as recent surgery or frequent travel.
Can dehydration increase my risk of blood clots?
Dehydration can increase your risk of blood clots by thickening your blood. Staying well-hydrated is one way to help prevent the development of a blood clot in the ankle while keeping the vein walls from narrowing.
Is an ankle blood clot more common after long travel?
Ankle blood clots are more common after long travel. Prolonged sitting during flights can slow down blood circulation, potentially leading to the formation of clots. Individuals with severe vein disease or a history of DVT may face greater discomfort or risk while flying and should take extra precautions.
Can swollen ankles cause blood clots?
Swollen ankles do not cause blood clots, but they can lead to symptoms that increase the risk of them forming. A blood clot in the ankle can cause persistent swelling, accompanied by other symptoms such as redness or unusual warmth.