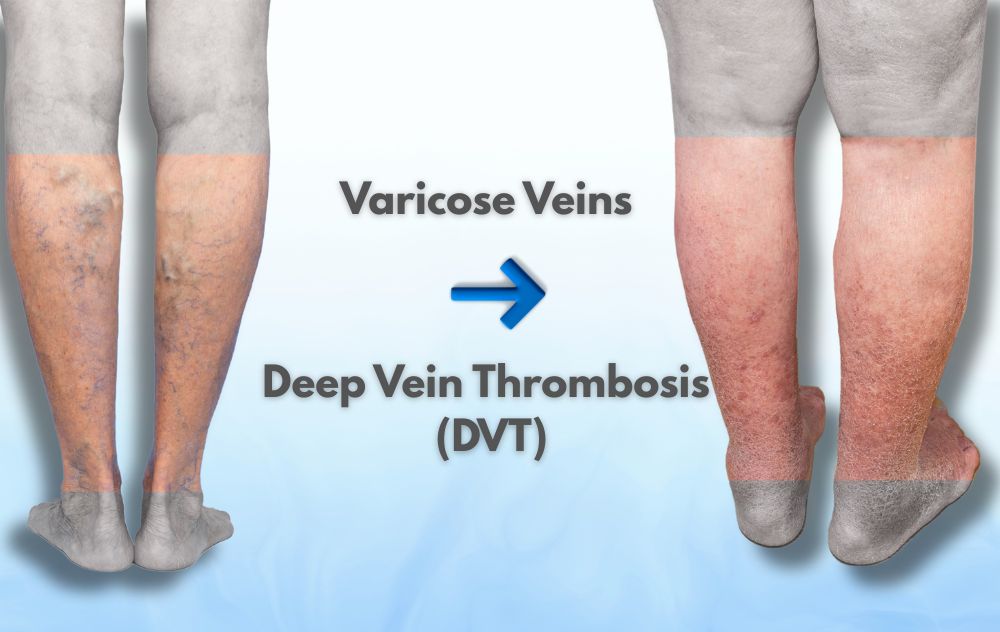
Varicose veins affect more than 30 million Americans and are often dismissed as a cosmetic issue. But for many patients, leg pain, swelling, or visible veins raise a deeper concern:
Can varicose veins turn into deep vein thrombosis (DVT)?
The answer is nuanced and important. While varicose veins and DVT are not the same condition, untreated or advanced vein disease can increase your risk of dangerous blood clots under certain circumstances. Understanding how these conditions are connected and when symptoms become serious can help protect your long-term health.
Varicose veins do not directly turn into DVT, but severe or untreated varicose veins can increase your risk of developing blood clots, especially when combined with factors such as immobility, inflammation, superficial thrombophlebitis, or chronic venous insufficiency (CVI).
This is why persistent or worsening symptoms should never be ignored.
Concerned about blood clots, leg pain, or swelling? A simple, non-invasive ultrasound can help rule out DVT and identify underlying vein disease.
Schedule a vein evaluation online
What Is Deep Vein Thrombosis (DVT) and Why It’s So Serious
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, most commonly in the legs. These veins carry a large volume of blood back to the heart, which is why clots in this system are medically dangerous.
If a clot breaks loose, it can travel to the lungs and cause a pulmonary embolism (PE) a life-threatening emergency that requires immediate treatment.
Why doctors take DVT seriously:
- Clots restrict or block blood flow
- Risk of pulmonary embolism if the clot migrates
- Can lead to chronic complications such as post-thrombotic syndrome
- May cause long-term leg pain, swelling, and skin damage
Early detection significantly reduces these risks.
Pulmonary Embolism (PE) Symptoms Many People Don’t Connect to Leg Clots
Many people search for leg pain, calf cramps, or swelling without realizing that breathing symptoms may signal a blood clot has traveled from the leg to the lungs, a condition known as pulmonary embolism (PE).
A pulmonary embolism occurs when part of a deep vein clot breaks loose and blocks blood flow in the lungs. This can reduce oxygen levels in the body and place sudden strain on the heart. In some cases, PE symptoms appear before leg symptoms or occur without noticeable leg pain at all, which is why they are often overlooked.
Seek emergency medical care immediately if you experience:
- Sudden shortness of breath or difficulty breathing at rest
- Sharp or worsening chest pain, especially when taking a deep breath or coughing
- Rapid or irregular heartbeat (heart racing or pounding)
- Lightheadedness, dizziness, or fainting
- Coughing up blood
These symptoms can develop with or without leg swelling or pain and should never be ignored. Pulmonary embolism is a life-threatening condition, but prompt treatment can be lifesaving.
Important note: If you have a history of varicose veins, recent surgery, prolonged travel, or immobility, breathing symptoms should always be evaluated urgently.
What Are Varicose Veins and Why They’re More Than Cosmetic
Varicose veins develop when one-way valves inside leg veins weaken or fail, allowing blood to flow backward and pool instead of moving efficiently toward the heart. Over time, this increased pressure causes veins to enlarge, twist, and become visible beneath the skin.
Common symptoms include:
- Leg heaviness or aching
- Swelling in the ankles or calves
- Cramping or burning sensations
- Skin discoloration, dryness, or itching
Varicose veins affect the superficial venous system, which is different from the deep veins involved in DVT — but the two systems are connected, and problems in one can influence the other.
How Blood Clots Form When Circulation Slows
Blood clotting is a normal and essential process that helps stop bleeding after an injury. Under healthy conditions, your body carefully balances clot formation and clot breakdown to keep blood flowing smoothly.
Problems arise when clots form without an injury, usually because blood is moving too slowly or the vein walls become inflamed, a situation that commonly occurs in the legs.
Blood clots are more likely to form when:
- Blood flow becomes sluggish or stagnant, allowing clotting factors to concentrate
- Vein walls are inflamed or damaged, triggering the body’s clotting response
- Blood chemistry changes, making clotting more likely
When blood pools in the legs often due to varicose veins, chronic venous insufficiency (CVI), or prolonged immobility, it creates the perfect environment for unnecessary clot formation. Over time, this can lead to superficial thrombophlebitis or, in more serious cases, deep vein thrombosis (DVT).
This process explains why vein disease is not just a cosmetic concern, but a circulatory condition that can carry real medical risks when left untreated.
Superficial Thrombophlebitis: The Critical “Bridge” Between Varicose Veins and DVT
Superficial thrombophlebitis is an important vein condition that many patients and even some articles tend to overlook. It occurs when a blood clot forms in a superficial vein, most often within or near a varicose vein, triggering inflammation in the vein wall.
Although it affects veins closer to the skin rather than the deep venous system, superficial thrombophlebitis is not simply a benign or cosmetic issue.
Common symptoms of superficial thrombophlebitis include:
- Localized redness following the path of a vein
- Warmth and tenderness over the affected area
- A firm, cord-like structure felt just beneath the skin
- Pain that may worsen with standing or pressure
These symptoms can look mild at first, which is why the condition is sometimes dismissed or misinterpreted as routine varicose vein discomfort.
Why superficial thrombophlebitis matters medically
While superficial thrombophlebitis is not the same as deep vein thrombosis (DVT), it plays a crucial role in clot risk assessment because:
- It signals active inflammation and clot formation within the venous system
- In rare cases, the clot can extend into nearby deep veins, increasing DVT risk
- It indicates underlying circulatory stress, often linked to chronic venous insufficiency (CVI)
- It increases the need for medical surveillance, imaging, and follow-up
For many patients, superficial thrombophlebitis acts as a warning “bridge” condition, a sign that vein disease has progressed beyond cosmetic concerns and may now carry a higher risk of more serious clot-related complications if left untreated.
Early evaluation helps determine whether the clot is isolated or requires closer monitoring to prevent escalation.
Can Varicose Veins Increase Your Risk of DVT?
Yes , but indirectly.
Varicose veins alone rarely cause DVT. However, they are a visible sign of poor circulation and venous valve damage, which can increase clot risk when combined with other factors.
How varicose veins may contribute to clot risk:
- Sluggish blood flow: Blood pooling increases clotting potential
- Inflammation (phlebitis): Can lead to superficial thrombophlebitis
- Chronic venous insufficiency (CVI): Sustained pressure and inflammation
- Periods of immobility: Surgery, long flights, bed rest, or hospitalization
A large 2018 JAMA study found that individuals with varicose veins had a five-fold higher risk of developing DVT compared to those without varicose veins.
Important clarification:
Most people with varicose veins will never develop DVT but risk rises when vein disease is advanced or combined with additional risk factors.
Varicose Veins vs. DVT: Why Symptoms Can Be Confusing
| Feature | Varicose Veins | DVT |
|---|---|---|
| Affected veins | Superficial veins | Deep veins |
| Visibility | Often visible | Not visible |
| Pain | Aching, heaviness | Sudden, tight, deep pain |
| Swelling | Mild or gradual | Often sudden, one-sided |
| PE risk | Rare | High if untreated |
Because symptoms can overlap, imaging not guesswork is essential.
DVT Warning Signs You Should Never Ignore
Many people with varicose veins experience daily discomfort, which can make it difficult to recognize when symptoms signal something more serious. Deep vein thrombosis (DVT) often presents differently—and knowing these warning signs can be lifesaving.
Seek immediate medical attention if you notice:
- Sudden leg pain or cramping, especially in one calf that feels deep or tight rather than surface-level
- Swelling in one leg, particularly if it appears suddenly or worsens quickly
- Skin warmth or redness over part of the leg
- A persistent feeling of tightness, pressure, or heaviness that does not improve with rest or elevation
- Skin discoloration or tenderness when touching or walking
Unlike typical varicose vein discomfort, which often improves with elevation or movement, DVT symptoms tend to be sudden, one-sided, and progressively worse.
If these warning signs appear, do not assume they are part of routine vein disease. Prompt evaluation can prevent serious complications, including pulmonary embolism.
Shared Risk Factors That Increase Blood Clot Risk
Varicose veins alone rarely cause blood clots. However, the risk of deep vein thrombosis (DVT) rises when vein disease is combined with other medical or lifestyle factors that slow blood flow or increase clotting tendency.
Blood clot risk increases when varicose veins coexist with:
- Prolonged immobility, such as long-distance travel, recent surgery, hospitalization, or extended bed rest
- A personal history of blood clots or known clotting disorders
- Obesity, which increases pressure on leg veins and impairs circulation
- Pregnancy or recent childbirth, when hormonal and circulatory changes heighten clot risk
- Smoking, which damages blood vessels and increases inflammation
- Hormone therapy or birth control use, particularly estrogen-containing medications
The more overlapping risk factors present, the higher the importance of proactive evaluation and monitoring—even if symptoms seem mild.
Important reminder: Many blood clots are preventable when risk is identified early and circulation issues are addressed
How Vein Specialists Check for Blood Clots: Venous Duplex Ultrasound
The primary test used to detect blood clots is a Venous Duplex Ultrasound.
This non-invasive test:
- Visualizes blood flow in real time
- Detects clots in both superficial and deep veins
- Identifies venous reflux and CVI
- Requires no needles, contrast dye, or radiation
It’s fast, painless, and often performed during your first visit
If you’re unsure whether your symptoms are normal vein discomfort or something more serious, a venous duplex ultrasound can provide clarity.
Schedule a vein consultation to rule out DVT and identify underlying vein disease
When Should You See a Vein Specialist?
You should seek professional evaluation if:
- Varicose veins are worsening
- Leg symptoms interfere with daily life
- You’ve developed redness, swelling, or warmth
- You want to rule out blood clots or CVI
Early diagnosis doesn’t just reduce clot risk, it protects long-term vein health.
Schedule Your Consultation Online
Footnotes
-
Chang, S.L., et al. (2018). Association of Varicose Veins With Incident Venous Thromboembolism and Peripheral Artery Disease. JAMA





