Venous ulcers, or venous stasis ulcers, are chronic non-healing wounds that typically develop near the ankles when poor circulation prevents blood from flowing back up to the heart. They are often a symptom of vein disease and can be difficult to heal without proper treatment.
These ulcers may appear with symptoms such as swelling in the legs or ankles, cramps in the thighs or calves, and visible varicose veins. One of the primary differences between a venous ulcer and other types of chronic wounds is the manner in which they develop. Understanding the signs of venous stasis ulcers can help determine the appropriate treatment needed to relieve symptoms.
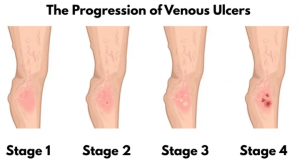
Venous Ulcer Stages
- Stage 1 – The start of a venous ulcer typically appears as red, inflamed skin. This stage usually goes undetected because venous ulcers resemble a bug bite, bruise, or mild irritation.
- Stage 2 – As the ulcer progresses, the inflamed skin may leak a small amount of fluid. This condition is more likely to be noticed at this stage, as the venous ulcer may look like a severe bruise, or the area may become reddened, dry, or cracked.
- Stage 3 – At this stage, the skin in the affected area begins to die. This is the foundation of the ulcer. Wounds will start to look inflamed and possibly deeper than before. Sometimes, venous ulcers may initially begin to heal but then reopen.
- Stage 4 – The open wound is visible and apparent. At this stage, it may not heal independently and must be kept clean to avoid infection.
What Does a Venous Stasis Ulcer Look Like?
If you are wondering what venous leg ulcers look like, it is essential to know that they can appear differently in the early stages. The appearance of a venous stasis ulcer evolves as it progresses.
In its early stages, it may present as a discolored area of skin, often reddish or purplish, which can be mistaken for a simple bruise or minor irritation. The skin in this area might also become thin, itchy, or feel firm and warm. This compromised skin can break down as venous insufficiency continues, forming a shallow wound. This initial ulcer might appear as a small, superficial sore with uneven or irregular edges and a red or pink base. Some may ooze clear fluid or develop a light crust.
Without proper management, the venous ulcer can worsen and enlarge. The base of the ulcer may deepen, and the surrounding skin can become increasingly discolored, often taking on a brownish hue due to hemosiderin deposits from blood leakage. The edges might become more defined, and the wound may produce more significant yellowish or greenish discharge, especially if an infection develops. Pain levels can also increase as the ulcer penetrates deeper tissues.
The venous ulcer can become quite large and deep in advanced or chronic stages, potentially exposing underlying tendons or bone. The surrounding skin is often significantly hardened and may exhibit a “woody” texture. Healing becomes challenging at this stage, and the risk of severe infections, such as cellulitis or osteomyelitis (a bone infection), is high. These non-healing ulcers can significantly impact quality of life and, in very severe, untreated cases, may lead to complications necessitating amputation.
Because a venous stasis ulcer can resemble other types of wounds, prompt medical evaluation is recommended. Ulcers, left untreated, can lead to serious complications, including infection and, in severe cases, tissue damage that can result in amputation.
CALL NOW TO SCHEDULE A VEIN SCREENING
Venous Ulcer Symptoms
The initial symptoms of venous ulcers are often overlooked or misdiagnosed, but as the ulcers progress, their symptoms become more recognizable. Venous stasis ulcers symptoms can include:
- Skin Discoloration: The skin around the ulcer may appear reddish-brown, purple, or discolored.
- Persistent Swelling or Aching: Noticeable swelling in the affected leg, especially around the ankle—also known as edema.
- Pain: Venous ulcers can be painful, particularly when standing or walking.
- Itching or Burning Sensation: Patients may experience itching or a burning sensation around the ulcer.
- Slow-Healing Open Sore: Venous ulcers typically heal slowly or not at all if left untreated.
- Foul Odor: The ulcer may have a foul odor due to infection or dead tissue.
- Discharge from the Wound: The ulcer may produce a clear, yellow, or greenish discharge.
- Changes in Skin Texture: The skin around the ulcer may look leathery with a thickened and hardened texture.
- Leg Fatigue or Heaviness: Sensation of heaviness or tiredness in their legs, especially after prolonged periods of standing or sitting.
What Causes Venous Stasis Ulcers?
Venous stasis ulcers are caused by underlying vein disease, which limits proper circulation and increases pressure in the veins. Over time, this can lead to inflammation, skin damage, and impaired healing, especially in the lower legs.
Venous Stasis Ulcer Risk Factors
Not everyone with vein disease will develop a venous leg ulcer, but certain health conditions and lifestyle factors can increase the likelihood.
Common venous stasis ulcers risk factors include:
- Family history of vein disease
- A sedentary lifestyle
- Aging
- Smoking
- Obesity
- High blood pressure
- Diabetes
- Varicose veins
- Pregnancy
- History of deep vein thrombosis (DVT) and other types of blood clots
While some risk factors, such as age or genetics, cannot be avoided, other factors can be managed through early intervention and expert guidance from a vein specialist. People with a history of deep vein thrombosis (DVT), in particular, are at increased risk due to the long-term damage that it can inflict on vein valves, often leading to chronic venous insufficiency (CVI).
Early intervention and ongoing support from a vein specialist are key to mitigating preventable risk factors and managing conditions like DVT and CVI, ultimately helping to preserve vein function and prevent more serious health issues such as venous ulcers.
Can Varicose Veins Cause Leg Ulcers?
Varicose veins can lead to venous leg ulcers due to increased vein pressure caused by blood pooling in the lower legs. This pooling, known as venous stasis, slows down blood flow and causes changes in the skin that make it more vulnerable to ulcer formation, especially around the ankles.
Treating the underlying venous issues through minimally invasive procedures is important for preventing and healing venous stasis ulcers. These vein treatments restore proper blood flow and reduce vein pressure, promoting better healing and reducing the risk of recurrence.
QUESTIONS? TALK TO A VEIN SPECIALIST
Treatment for Venous Ulcers
Venous stasis ulcer treatment focuses on addressing the underlying causes: chronic venous insufficiency, a form of vein disease. Without restoring healthy blood flow, ulcers often struggle to heal and are more likely to return.
USA Vein Clinics offers minimally invasive, non-surgical procedures to reroute blood flow away from damaged veins and toward healthy ones. These treatments improve circulation, reduce venous pressure, and create the right conditions for healing ulcers, even while the wound is still present.
A vein specialist possesses the specific knowledge and tools essential for:
- Accurate Diagnosis: They can precisely identify the extent of vein damage and the presence of conditions like CVI, often using specialized imaging techniques such as ultrasound.
- Tailored Management Plans: Vein specialists develop personalized strategies to manage your specific risk factors and address the underlying causes of venous disease. This might include conservative measures like compression therapy and lifestyle adjustments, or more advanced treatments.
- Specialized Treatment for DVT and CVI: For conditions like DVT and the resulting CVI, a vein specialist can offer a range of interventions, from medication management to minimally invasive procedures designed to improve blood flow, alleviate symptoms, and prevent further complications.
Our vein clinics offer the following minimally invasive procedures for treating the underlying cause of venous ulcers:
- Endovenous Laser Therapy (EVLT)
- ClariVein®
- Varithena®
- VenaSeal™
- Radiofrequency Ablation (RFA)
- Ultrasound-Guided Sclerotherapy (USGS)
- Visual Sclerotherapy
Treating the vein disease that causes venous ulcers is essential—not something to wait for until after the wound has healed. In fact, vein treatment often helps speed up healing when performed alongside proper wound care.
After vein treatment, many patients report reduced pain and swelling, improved mobility, better skin health, and a reduced risk of future ulcers recurring or serious complications, all contributing to a better overall quality of life.
Preventing and Managing Venous Ulcers
Maintaining healthy veins and promoting good circulation is crucial for preventing venous leg ulcers. Poor circulation in the legs—often caused by weakened vein valves—can lead to blood pooling, increased pressure, and eventually skin breakdown.
To lower your risk of developing venous stasis ulcers:
- Stay active and keep blood moving through your legs.
- Avoid long periods of sitting or standing without movement.
- Manage chronic conditions like diabetes, high blood pressure, and obesity.
- Wear compression stockings if recommended by your doctor.
- Elevate your legs when resting to encourage blood flow back to the heart.
- Keep conditions that exacerbate symptoms, like diabetes and high blood pressure, under control.
While venous stasis ulcers can often be treated successfully, the underlying vein disease cannot be reversed. Without ongoing care, ulcers may continue to progress or recur after healing. That’s why anyone with a history of venous leg ulcers or at risk of vein disease should monitor their condition carefully through regular examinations by a medical professional.
Get Relief from Venous Ulcers
USA Vein Clinics offers lasting solutions for venous stasis ulcers caused by vein disease. Our non-surgical treatments are performed in outpatient settings and require minimal downtime, allowing patients to return home and to normal activities the same day.
If you’re ready to alleviate symptoms of venous ulcers, call us at 888.768.3467 or schedule an initial consultation online using the link below.
Common Venous Ulcer FAQs
Why won’t my leg ulcer heal?
A leg ulcer that won’t heal can be caused by poor circulation, medical conditions such as venous insufficiency, infection, or inadequate wound care. If a leg ulcer doesn’t improve within a few weeks or shows signs of infection, seek medical attention to prevent serious complications.
Do venous stasis ulcers affect both legs?
Venous stasis ulcers typically develop due to venous insufficiency, which can affect one or both legs. While it’s common for one leg to be more severely affected, the condition can progress and lead to ulcers on both legs, especially if left untreated.
Do venous ulcers come back after healing?
Venous leg ulcers can recur after healing, particularly if the underlying issue of venous insufficiency is not treated.
Schedule Anytime, Anywhere
Skip the wait times! Scheduling at your fingertips, 24/7. Minimally invasive non-surgical treatment for spider & varicose veins.
Schedule Online